Author: Brit Long, MD (@long_brit) // Reviewed by: Alex Koyfman, MD (@EMHighAK)
The American Heart Association released an updated scientific statement on management of elevated blood pressure. This post will provide the key points for emergency clinicians.

Background
Hypertension (HTN) is significant issue globally and a leading risk factor for cardiovascular disease. HTN was the primary diagnosis in over 1 million ED visits in 2023, and rates of HTN emergencies have increased over the past 20 years. From 2006-2013, HTN emergencies occurred in approximately 2 of every 1000 adult ED visits. While mortality of HTN emergency has decreased, rates range from 0.2-11%.
Asymptomatic elevated BP is more common than HTN emergencies and is present in up to 78% of patients at admission. Risk factors for elevated BP include older age, Black adults, diabetes, chronic kidney disease, and cerebrovascular disease.
Classification
Elevated BP in the inpatient setting can be classified as asymptomatic elevated BP versus HTN emergency (elevated BP with signs of new or worsening target-organ damage).
Importantly, there is no “hypertensive urgency”.
The AHA defines elevated inpatient BP as SBP > 130 or DBP > 80 mm Hg.
If SBP is < 180 and DBP is < 110 mm Hg, that is asymptomatic elevated BP.
If SBP is > 180 or DBP is > 110-120 mm Hg and the patient has no new/worsening target organ damage, that is asymptomatic markedly elevated BP.
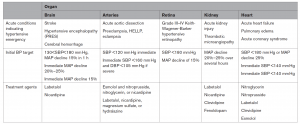
However, ff SBP is > 180 or DBP is > 110-120 mm Hg and the patient does have new or worsening target organ damage, the patient has HTN emergency. BP related target organ damage includes any harmful effects/injuries to the brain (hypertensive encephalopathy, intracranial hemorrhage, acute ischemic stroke), heart (acute myocardial infarction, unstable angina, acute left ventricular failure with pulmonary edema), large vessels (dissecting aortic aneurysm), kidneys, and the microvasculature (high-grade retinopathy, acute kidney injury, or microangiopathic hemolytic anemia and thrombocytopenia). This can be recalled with the “BARKH”acronym (brain, arteries, retina, kidney, heart).

BP Measurement in the Acute Care Setting
BP recordings depend on the device type, validation and calibration of the device, BP cuff size and placement, patient position, and other factors (patient anxiety, pain, blood draws, etc.).
When measuring BP, ensure the right-sized BP cuff and technique are used.
For patients with HTN emergencies and for those receiving intravenous antihypertensive medications, arterial lines are preferred for accuracy and to avoid false readings.
Management of Elevated BP
Treatment of the patient with elevated BP first involves determining whether the patient has HTN emergency versus asymptomatic HTN. The BP measurement technique should be assessment, as should the reading severity, causes of elevated BP, evaluation for target organ damage, and determining the risks versus benefits of starting antihypertensive medications.

If the patient has asymptomatic elevated BP, the optimal management strategy is not clear, and there are no data that treating asymptomatic elevated BP (marked versus not) in the acute care setting improves clinical outcomes. Observational studies suggest acutely treating asymptomatic inpatient hypertension is associated with harm, and they strongly recommend against this practice. Administration of IV antihypertensives in the absence of HTN emergency is not recommended.
Rather than administrating antihypertensives in the patient with asymptomatic elevated BP, factors such as the technique and site of the BP cuff, time of day (BP higher at evening), patient pain/anxiety/sleep deprivation, other medications (steroids, fluids), illicit substance use must be considered.
In the ED setting, they recommend avoiding intensifying HTN medications. The ED clinician should treat any condition that may be contributing to the elevated BP, with a preference towards restarting home medications and ensuring the patient is aware of their elevated BP and the need for follow-up.
The AHA Scientific Statement recommends the A-I-M approach (Assess, Identify, Modify) for HTN.

Of note, they caution against lowering the BP of patients with asymptomatic markedly elevated BP prior to going to the hospital floor, as this is not evidence based and furthers the myth that treatment of the BP is necessary. Overtreatment can result in patient harm.
HTN Emergency
If the patient has target end organ damage with markedly elevated BP, HTN emergency is present, and the BP should be emergently reduced based on established algorithms. Specific antihypertensives and BP targets are based on the organ affected.
AHA Key Implications for Clinical Practice

Reference: