Welcome back to the “52 in 52” series. This collection of posts features recently published must-know articles. Our fifteenth post looks at terminal QRS distortion in determining benign early repolarization versus ischemia.

Author: Christiaan van Nispen, MD (Emergency Medicine Physician Resident, San Antonio, TX) and Brannon Inman (Chief Resident, Emergency Medicine Physician, San Antonio, TX) // Reviewed by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Terminal QRS distortion is present in anterior myocardial infarction but absent in early repolarization
Clinical question:
When the differential diagnosis for precordial ST segment elevation (STE) is benign early repolarization versus ischemia, is the presence of terminal QRS distortion (TQRSD) specific to ischemia?


Study design:
- Secondary analysis of retrospective data
PICO:
Population:
- Patients presenting with chest pain at an urban, level 1 trauma center with full revascularization capabilities and ED annual census of 95,000 patients
- Reviewed electrocardiogram (ECG) database of all chest pain patients over a 2.5 year period with cardiologist confirmed the interpretation of benign early repolarization
- Included: all ECGs of patients with non-ischemic final diagnosis after 3 serially negative cardiac troponins
- Excluded: lack of at least 1-mm STE in any of V2-V4

Intervention:
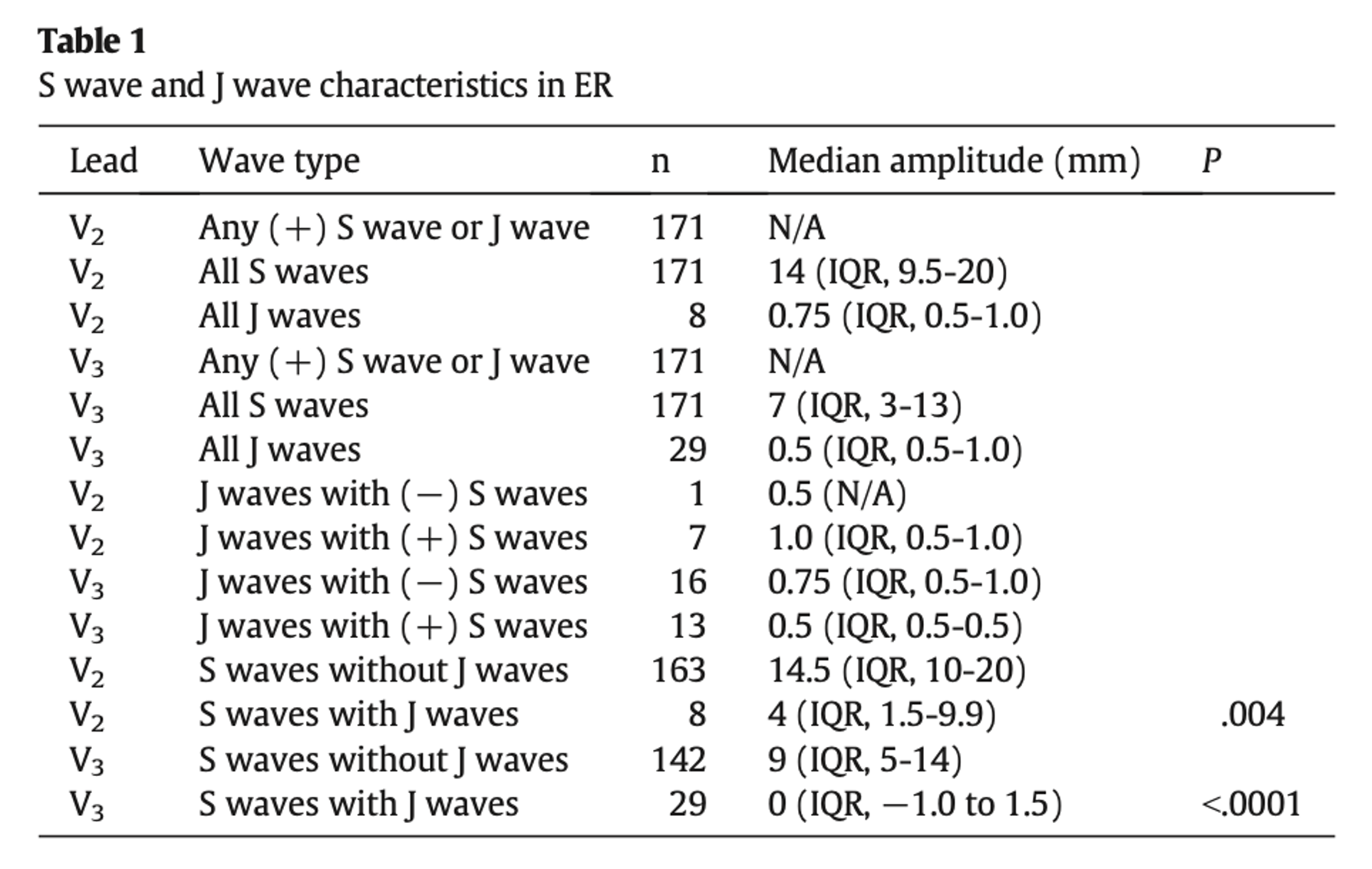
- Included ECGs were scrutinized for the presence of TQRSD (the absence of both S wave and J wave in at least one of leads V2 or V3)
Comparator: None
Outcome:
- Of 171 benign early repolarization ECGs included, all 171 had at least one of S wave or J wave in at least V2 or V3and thus did not meet criteria for TQRSD
- In lead V2, 1 out of 171 lacked S wave but did have a J wave in V2
- In lead V3, 16 out of 171 lacked S wave, but all did have a J wave in V3
Take Aways:
- ECGs that were diagnosed as BER by a cardiologist were examined for the presence of TQRSD. Of the ECGs examined, none had TQRSD.
- The study only included patients with at least 1mm of ST elevation.
- This study examined leads V2 – V4 for the presence of TQRSD.
- Of the 171 ECGs examined, the median age was fairly young: 38 years in males and 24 years in females. These are the patients I would expect to see more BER in and less acute MI. Furthermore, these are patients who had already been diagnosed with BER and have had serial negative troponins, leading to a low pre-test probability of acute MI.
- Of the patients excluded for ‘obvious’ left anterior artery occlusion, several ECGs were not able to be analyzed, so we don’t know the true presence of TQRSD in these patients.
- The use of only one physician to review ECGs exposes the study to inter-rater reliability issues (the second reviewer was a medical student).
My Take:
This is a secondary analysis of a prior retrospective suggesting that TQRSD is an uncommon ECG pattern in BER. Based on this study, TQRSD in a patient with concerning history and exam warrants consideration of acute coronary occlusion.
Reference:
Lee DH, Walsh B, Smith SW. Terminal QRS distortion is present in anterior myocardial infarction but absent in early repolarization. Am J Emerg Med. 2016;34(11):2182-2185. doi: 10.1016/j.ajem.2016.08.053






