Welcome back to the “52 in 52” series. This collection of posts features recently published must-know articles. Post #26 looks at oxygen targets in the post-ROSC patient after OHCA.

Author: Dan O’Conor, MD (Resident, Emergency Medicine Physician, San Antonio, TX) and Brannon Inman, MD (Chief Resident, Emergency Medicine Physician, San Antonio, TX) // Reviewed by: Alex Koyfman, MD (@EMHighAK); and Brit Long, MD (@long_brit)
Effect of Lower vs Higher Oxygen Saturation Targets on Survival to Hospital Discharge Among Patients Resuscitated After Out-of-Hospital Cardiac Arrest
AKA: The EXACT Randomized Clinical Trial
Question:
In patients with out of hospital cardiac arrest (OHCA) from a presumed cardiac cause who have obtained return of spontaneous circulation (ROSC), does targeting a lower oxygenation saturation in the early phase of post-ROSC care improve survival?
Study design:
- A multi-center parallel-group block-randomized controlled trial
- Patients and outcome assessors blinded

PICO:
Population:
- Included patients in 2 EMS systems and 15 hospitals in Victoria and South Australia, Australia from December 11, 2017- August 11, 2020
- Included adult patients (above age 18) with OHCA from presumed cardiac cause with subsequent ROSC
- Additional inclusion criteria:
- unconscious after ROSC
- advanced airway (endotracheal tube or supraglottic airway)
- transport planned to a participating hospital
- maintained SpO2 >95% while receiving 10L/min supplemental O2 or FiO2 100%
- Exclusion criteria:
- Pregnancy
- Evidence of non-cardiac cause of arrest
Intervention:
- Oxygen restriction: Supplemental oxygen titration prior to ICU arrival to achieve SpO2 90-94%
Comparator:
- Liberal oxygen: Supplemental oxygen titration prior to ICU arrival to achieve SpO2 98-100%
Outcome:
- No significant difference in the primary outcome (survival to hospital discharge)
- Statistically significant increased risk of hypoxic episodes (SpO2 <90%) in the intervention group


Randomization:
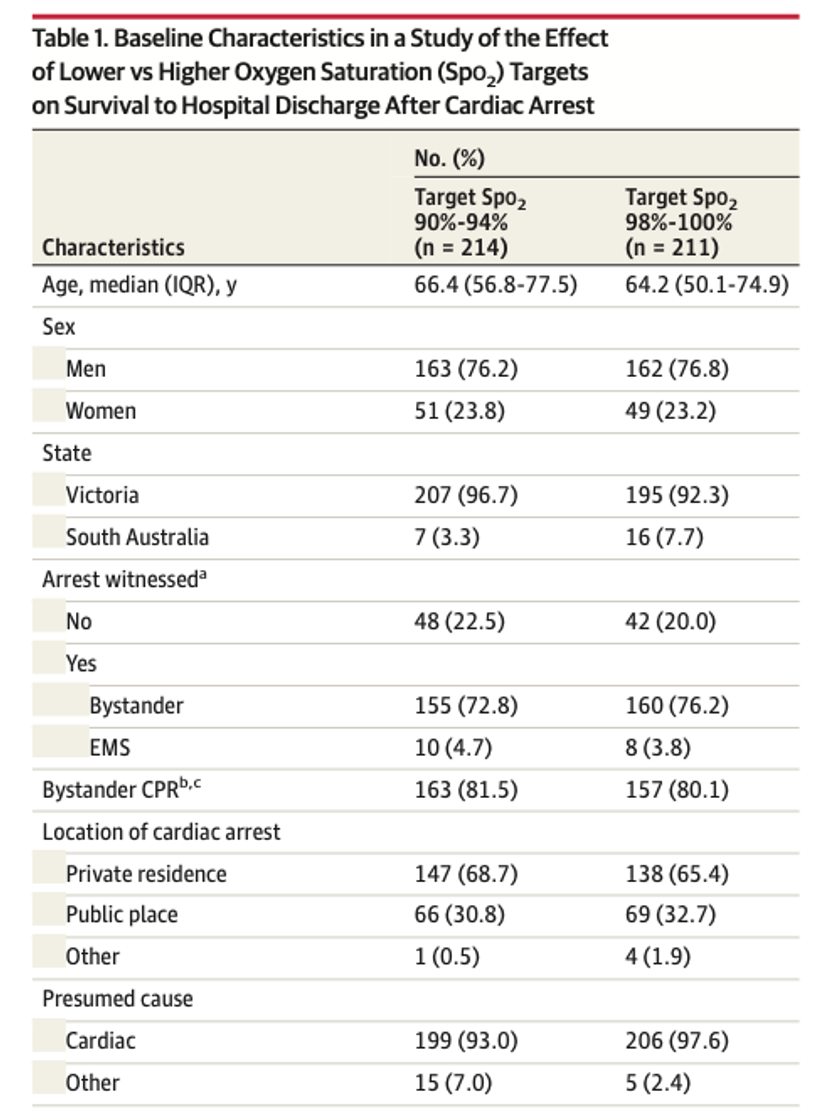
- Treatment arms were fairly well-balanced.


Take away:
- This was a negative trial, although it was limited by early termination prior to target enrollment due to the COVID pandemic.
- There were increased rates of sustained hypoxia in the intervention group, although this “adverse effect” is an oxygen range immediately adjacent to the target range.
- Strengths:
- This study includes patient-oriented outcomes and outcomes that are directly related to the hypothesized mechanism (CPC neurologic assessment scale as a secondary outcome when the premise is that standard care causes reperfusion brain injury).
- This study contrasts with prior preliminary studies suggesting a benefit of conservative oxygen strategies.
- Authors note that the precise oxygen titration was difficult with the equipment available pre-hospital.
- Mean SpO2 in the intervention group was 97% (range 94-99%) at ED arrival despite a goal of 90-94%.
- This decreases the likelihood that if a difference exists between groups that it could be detected by this study, although there was a noticeable difference in PaO2 at ED arrival.
- Median 95mmHg in the intervention group vs 130mmHg in the standard group without any PaO2 <60 in the intervention group which suggests that hyperoxia was in fact mitigated in the intervention group without causing hypoxia.
- The only subgroup in which survival varied was patients with or without bystander CPR. This may support the theory that patients with shorter downtime/hypoxia are at less risk of hypoxia and therefore do not stand to benefit as significantly from measures aimed to reduce reperfusion injury. This should be viewed as hypothesis-generating at this stage.
My take:
I will not intentionally target hyperoxia, and it is not clear whether 90-94% is inferior or superior to 98-100% based on this trial. There is likely a greater number of desaturation episodes when targeting 90-94%, but it is not clear this is associated with patient harm.
Reference:
- Bernard SA, Bray JE, Smith K, et al. Effect of Lower vs Higher Oxygen Saturation Targets on Survival to Hospital Discharge Among Patients Resuscitated After Out-of-Hospital Cardiac Arrest: The EXACT Randomized Clinical Trial. JAMA. 2022;328(18):1818-1826. doi:10.1001/jama.2022.17701







1 thought on “52 in 52 – #26: The EXACT Trial”
Pingback: Quiz 178, February 3, 2023 – The FOAMed Quiz