52 in 52 – #40: DIRECT MT – Endovascular Thrombectomy with or without Intravenous Alteplase in Acute Stroke
- Aug 10th, 2023
- Brannon Inman
- categories:
Welcome back to the “52 in 52” series. This collection of posts features recently published must-know articles. Today we look at the DIRECT MT trial.

Author: Brannon L Inman, MD (Critical Care Fellow, Orlando, FL) // Reviewed by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Endovascular Thrombectomy with or without Intravenous Alteplase in Acute Stroke
AKA: The “DIRECT MT” Trial
Clinical question:
In patients with anterior circulation large vessel occlusion, is thrombectomy alone non-inferior to thrombectomy preceded by alteplase?
Study design:
- Multicenter open label randomized control trial
- Enrolled patients from 41 tertiary care hospitals in China
- Assessing for statistically significant difference in modified Rankin score at 90 days
PICO:
Population: 206 patients were enrolled with 107 in the intervention group and 99 in the control.
– Inclusion criteria:
- Enrolled patients over the age of 18 with acute ischemic stroke with CTA confirmed occlusion of ICA, or M1 or M2 segment of MCA
- Within 4.5 hours of onset
- Eligible for tPA and thrombectomy
- NIHSS ≥ 2
– Exclusion criteria:
- Disability before presenting CVA, defined by modified Rankin score ≥2
- Any contraindication of IV tPA or thrombolytics

Randomization:
- Slightly longer median duration in tPA group (167 vs 177)
- Overall very similar in terms of group baseline characteristics

Intervention:
- Endovascular thrombectomy alone
Comparator:
- Endovascular thrombectomy + tPA
Outcome:
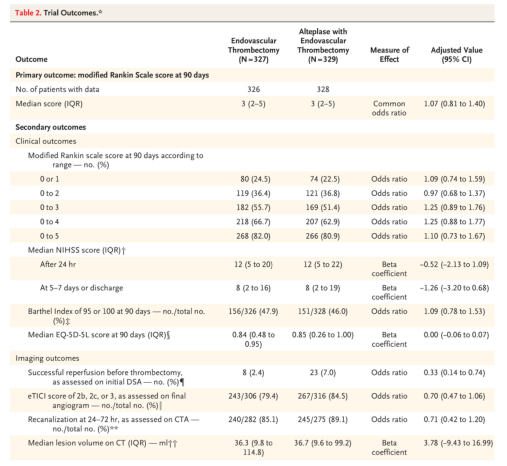
- No statistically significant difference in primary outcome
- mRS 3 (2-5) vs 3 (2-5)
- Adjusted value 1.07 (95% CI 0.81-1.40)
- No statistically significant difference in secondary outcomes
- No significant difference in safety outcomes
- Death 18% vs. 19%, RR 0.94 (0.68-1.30)
- Intracranial hemorrhage
- Asymptomatic 33% vs. 36%, RR 0.92 (0.75-1.14)
- Symptomatic 4% vs. 6%, RR 0.70 (0.36-1.37)
- Infarction in new territory at 5-7 days 3% vs. 3%, RR 1.23 (0.52-2.93)
- Large or malignant MCA infarction 13% vs. 13%, RR 0.98 (0.66-1.46)
- Any procedural complication 15% vs. 14%, RR 1.05 (0.72-1.52)
Take away:
- This trial found no significant difference in thrombectomy alone versus thrombectomy plus alteplase.
- It was a well-conducted multicenter trial. However, given the monochromatic study population there is limited external validity and generalizability, particularly in more heterogeneous patient populations.
- While patients had to be within 4.5 hours to be randomized, the median IQR was 7 hours (4-12) to start of tPA for the control group. This raises concern that patients may have received tPA after 4.5 hours of stroke onset. Based on the data current guidelines lean on, this could raise concern about the expected validity of the tPA therapy (i.e., these patients may have received tPA too late for it to be even plausibly useful).
- Based on the times from tPA to arterial puncture and door to puncture times, this study only really applies tocomprehensive stroke centers with thrombectomy capability. These data cannot be applied to centers that have to transfer patients to higher levels of care.
My take:
It’s entirely possible that in comprehensive stroke centers tPA may confer no added benefit to thrombectomy for anterior circulation LVOs. However at the bedside based on current guidelines, I will continue to offer tPA when indicated or requested by endovascular operators.
Reference:
- Yang P, Zhang Y, Zhang L, et al. Endovascular Thrombectomy with or without Intravenous Alteplase in Acute Stroke.N Engl J Med. 2020;382(21):1981-1993. doi:10.1056/NEJMoa2001123
