Introduction
- Over 10% of US population has some form of chronic kidney disease (CKD), and more than 350,000 persons require hemodialysis for end stage renal disease (ESRD) annually.1
- Within the next decade, the incidence of CKD is expected to nearly double.1
- Uremic bleeding is a well-known consequence of CKD and can result in significant morbidity and mortality.
Why Do Uremic Patients Bleed?
- No one substance has yet to be identified as the cause of uremic bleeding and the bleeding is likely to be multifactorial.
- Uremic toxin accumulation causes a disruption of von Willebrand Factor (vWF), which leads to platelets’ inability to bind.
- This means that typical coagulation studies on uremic bleeding patients (PT, PTT) will be normal.
- Bleeding time is an indirect measure of platelet function and is almost always elevated.
- Stage of kidney disease does not correlate well with bleeding risk.2
Why is Bleeding a Concern in this Population?
- A normocytic normochromic anemia is present as early as stage 3 CKD and is almost universal by stage 4.1 An anemia of chronic disease picture may also be seen.
- These anemias are mainly due to the diseased kidney’s inability to adequately produce erythropoietin (EPO).
- Despite the defective nature of platelets described above the platelet count is usually normal.
Presentations of Uremic Bleeding
| Petechiae |
| Epistaxis |
| Bleeding following invasive procedure (such as catheter placement): Dialysis access site hemorrhage typically occurs in the setting of aneurysms, anastomosis rupture, or over-anticoagulation.4 |
| Hemorrhagic pericarditis |
| Hemorrhagic pleural effusion |
| GI hemorrhage: Hemorrhage of the upper gastrointestinal tract is the second leading cause of death in patients with acute renal failure.3 |
| Intracranial Bleed: Subdural hematomas can mimic dialysis disequilibrium syndrome |
| Retroperitoneal bleed: Consider hemorrhage into renal cysts in the undifferentiated hypotensive ESRD patient |
| Spontaneous subcapsular hematoma of the liver |
| Ocular hemorrhage |
| Uterine hemorrhage |
Treatment
General goals for treatment
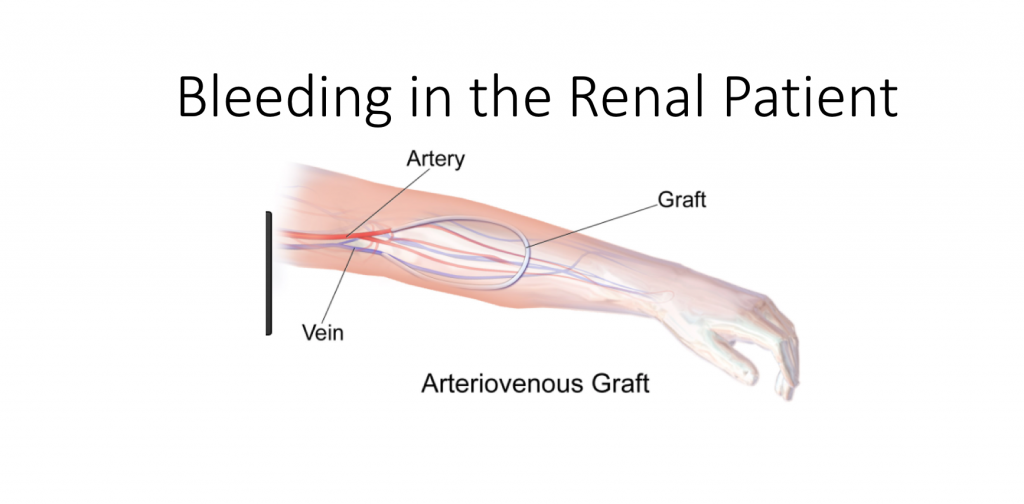
- A patient’s dialysis access is their lifeline, and its compromise should only occur if their life is in jeopardy.
- Patients with ESRD on dialysis have very delicate fluid balance and fluid overload may be apparent on aggressive resuscitation.
Direct pressure
- Avoid placing a suture into a graft or fistula unless absolutely necessary.
- A single stitch will often work better if there is a linear tear in the access site versus a puncture.
- A tourniquet will stop the flow from a bleeding access site on the extremity but will most surely result in thrombosis of the graft or fistula.
Dialysis
- Difficult in the actively bleeding patient
- Avoid heparin
- Corrects bleeding time in 65-85% of patients
- In general, peritoneal dialysis patients have less bleeding risk than hemodialysis patients.
**Desmopressin / DDAVP
- Mechanism of action not fully known: likely increases the release of factor 8 VWF polymers from the vascular endothelium => improves platelet aggregation.
- Effective in about 50% of patients
- Dose: 0.3 mcg/kg SC or IV; onset: 1 hour; duration: 4-8 hours
- 1 dose can lead to tachyphylaxis secondary to depletion of factor VIII and vWF from endothelial stores.3
- Contraindications: polydipsia, unstable angina, or severe congestive heart failure due to its antidiuretic effect
- Special considerations: if no IV access DDAVP can be administered intranasally at a dose of 3 mcg/kg, however IV dose is preferred.
Protamine
- Heparin is frequently used during dialysis. The half-life of heparin is short (1.5 hours), thus Protamine will only be effective during the first few hours.
- Dose: 1 mg of Protamine for every 100 units of heparin given. If the heparin dose is unknown, 10-20 mg of protamine can be given.4
- Contraindications: Avoid in fish allergy, caution if prior vasectomy and caution in pulmonary hypertension
Estrogen
- Rarely useful in ED setting, onset: 1 day
Topical Hemostatic agents
Helpful when bleeding from dialysis access site.
| Gelatin products |
|
| Thrombin |
|
Cryoprecipitate
- Contains Factor VIII, fibrinogen, Factor XIII, vWF, and fibronectin
- Dose: Use 10 bags of Cryoprecipitate over 30 mins; should see an effect within 4-12 hours6
Platelet Transfusion
- Only in cases of uncontrolled hemorrhage
- Platelets become dysfunctional shortly after entering uremic environment
- Use in combination with other agents (i.e. desmopressin, cryoprecipitate, and packed red blood cells).3
*Packed RBCs
- Transfuse to a level of around 10mg/dl; ensure that this is given along with DDAVP and platelets +/- cryoprecipitate.
- Remember, anemia worsens bleeding
For an algorithm on the management of uremic bleeding, check out “Evidence-based treatment recommendations for uremic bleeding” published in Nature.2
Further Reading
- Bargman J.M, Skorecki K. Chronic Kidney Disease In: Harrison’s Principles of Internal Medicine. 16th ed. New York, NY: McGraw-Hill; 2011:2308
- Hedges, S.J ET al. Evidence-based treatment recommendations for uremic bleeding. Nature Clinical Practice Nephrology 2007 March; 3(3):138-153
- Venkat A., Kaufmann K.R., Venkat K.K., Care of the end-stage renal disease patient on dialysis in the ED. The American Journal of Emergency Medicine (2006) 24, 847 – 858
- Larsen, C., Weathers B, Schwartzwald, M, and Barton, M.A. Focus On: Dialysis Emergencies. American College of Emergency Physicians 2010 October
- Berry G.W., Griffin D.L., and Schraga E.D. Topical Hemostatic Agents. Medscape 2013 May
- Cryoprecipitate @ Life in the Fast Lane
- Salsman S. Uremic Bleeding: Pathophysiology, Diagnosis, and Management. Hospital Physician 2001 May; 76 45-50.
- Mannucci, M. Desmopressin (DDAVP) in the Treatment of Bleeding Disorders: The First 20 Years. Blood 1997 October 90(7): 2515-2521.
- Spontaneous retroperitoneal hemorrhage in a dialysis patient.






1 thought on “Bleeding in the Patient with Renal Failure”
Pingback: Asynchronous Learning: Renal and Urogenital Emergencies - Bold City Emergency Medicine