Originally published at CoreEM.net, dedicated to bringing Emergency Providers all things core content Emergency Medicine available to anyone, anywhere, anytime. Reposted with permission.
Follow Dr. Swaminathan and CORE EM on twitter at @EMSwami and @Core_EM
Written by Vibha Gupta, MD and Edited by Anand Swaminathan, MD
Definition: Malfunction, dislodgement or bleeding complication related to a tracheostomy
Background
- Tracheostomies are performed more commonly than laryngectomies
- Stoma tract is considered mature after 7 days
Indications for tracheostomy (Mcgrath 2012)
- Bypass glottic or supraglottic stenosis/obstruction
- Access for tracheal toilet
- Provision of a more comfortable airway for prolonged ventilation
- Protection from aspiration
Common Complications (Engels 2009)
Complications can be immediate, short term or long term after placement
| Immediate Complications (hours) | Short-Term Complications (< 7 days) | Long-Term Complications (> 7 days) |
|---|---|---|
| Paratracheal Insertion | Bleeding | Tracheomalacia |
| Posterior Tracheal Wall Laceration | Accidental Decanulation | Tracheal Stenosis |
| Infection | Tracheo-esophogeal Fistula | |
| Loss of Airway | Tracheoarterial Fistula | |
| Subcutaneous Emphysema | Erosion | |
| Aspiration | Vocal Cord Paralysis | |
| Delayed Stoma Closure |
Basic Anatomy
- A patient with a tracheostomy likely has an anatomically challenging which often resulted in the tracheostomy being performed (i.e. tumor, obstructive sleep apnea) as well as due to the complications which can arise from the procedure itself
- A review of the relevant anatomy
- Tracheostomy is placed inferior to the cricothyroid membrane
- Common location: between the second and third tracheal rings
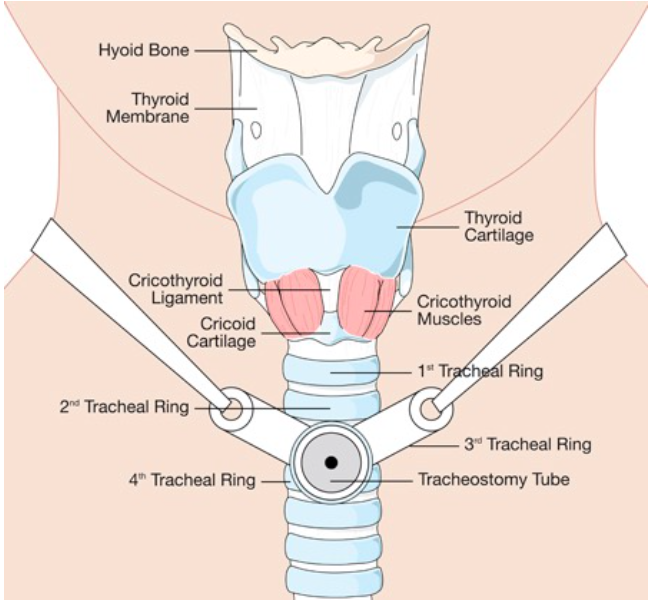
Tracheostomy Basic Anatomy (pinimg.com)
Signs + Symptoms of Tracheostomy Problems
- Hypoxia
- Difficulty breathing
- Inability to suction
- Inability to place inner cannula
- Bleeding
- Swelling
Pertinent history
- When was the tracheostomy performed? (>7 days for safe exchange of tubing)
- What was the tracheostomy indication?
- Recent tracheostomy changes/downsizing?
- Recent hospitalizations or infections?
- Is patient taking anticoagulation?
- Any symptoms of fever, cough, increased sputum production?
ED Approach to Management (Mcgrath 2012)
Consider Common Complications
- Displacement of the tube
- Obstruction of the tube
- Equipment malfunction
- Bleeding
- Infection

Tracheostomy Tube (www.practicalslpinfo.com)
Bedside Equipment
- Personal protective equipment
- Suction (2 suction canisters, with inline suction available)
- Trachestomy equipment – one the same size, one tube a size smaller
- Oxygen bag and mask
- LMA
- Laryngoscope with ETT (6.0, 7.0, 7.5)
- Capnography
- Bougie (may be needed to aid in exchanging tracheostomies in the setting of swelling, bleeding etc
Assesment of Breathing
- Listen, look and feel for evidence of breathing at the native upper airway and over the tracheostomy site for 10 seconds
- End tidal CO2 waveform capnography
- Pulse oximetry
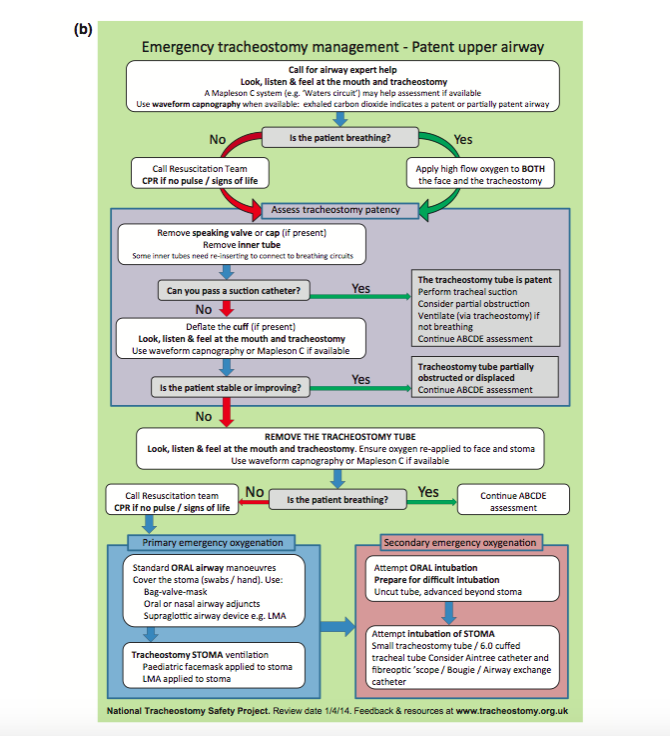
Emergency Tracheostomy Management (Mcgrath 2012)
- Assessment
- Remove inner cannula, speaking valve, humidifying device
- Look with a fiberoptic scope if there is one available
- Attempt to pass a suction catheter- if it passes then tube is patent, if not you know it is blocked or displaced
- Deflate the cuff. Sometimes, the extra room from deflating the cuff allows the patient to ventilate on their own.
- Some tracheostomy issues will go beyond your level of expertise
- Particularly important in patients with new (< 7 days) tracheostomies where simple exchange may not be possible due to immaturity of the tract
- Call for Surgical Backup (ENT, General Surgery, Anesthesia) Early
- Obstruction/displacement
- If obstructed or displaced and unable to ventilate- must remove and replace tracheostomy
- Can use a smaller diameter tracheostomy tube to replace the current tube using a bougie or fiberoptic scope
- If track is immature (< 7 days old) blind replacement is contraindicated
-
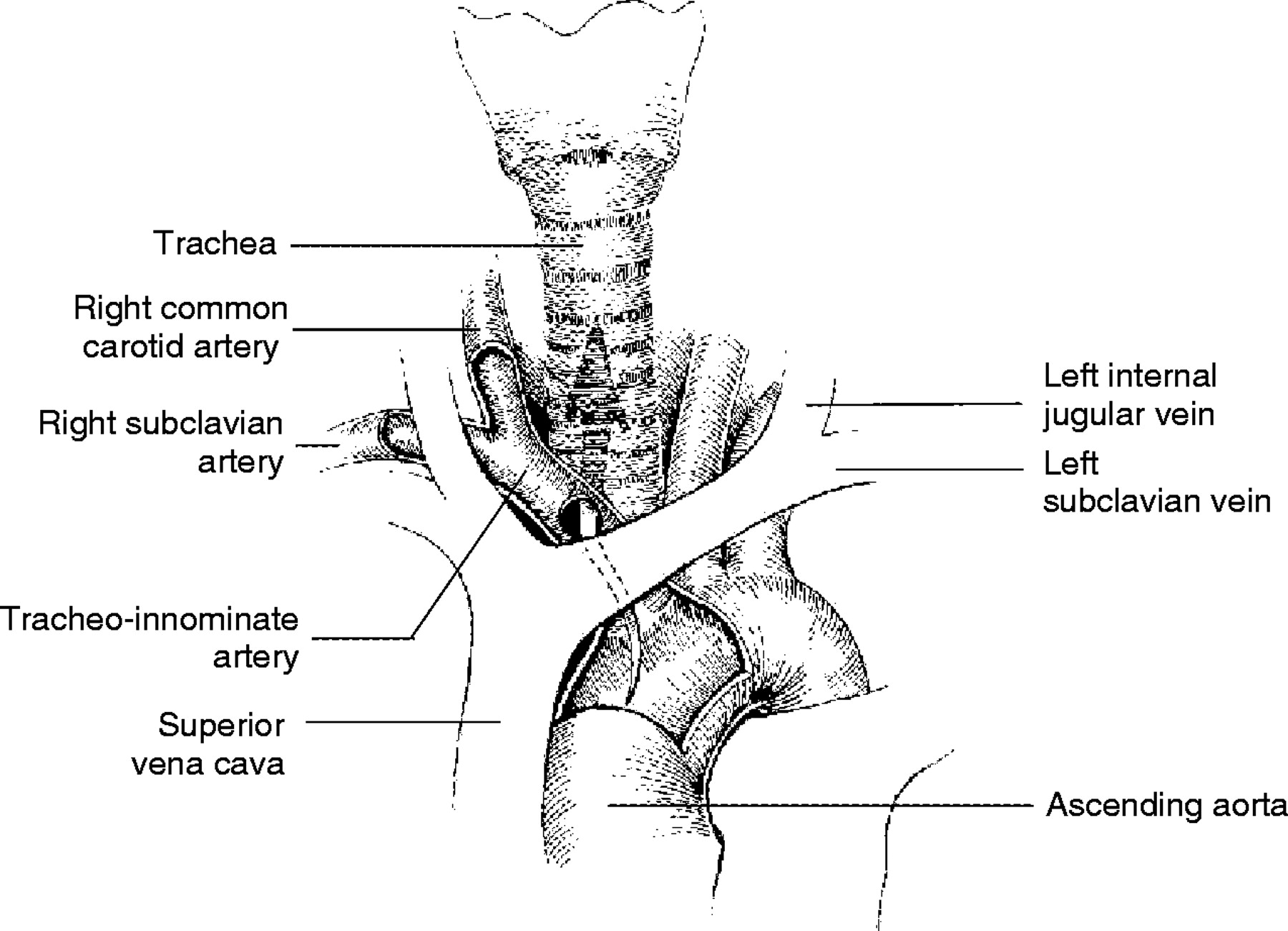
Tracheo-innominate Fistula (crashingpatient.com)
Bleeding from the tracheostomy
- Herald bleed in tracheo-innominate fistula: small self-resolved bleeding that is harbinger of subsequent bleeding
- 50 % of cases have a herald bleed prior to a massive bleeding event (Grillo 2003)
- Even minor bleeding warrants evaluation in an OR setting with bronchoscopy. If flexible bronchoscopy is unrevealing then rigid bronchoscopy should be performed (Ailiwadi 2009)
- Causes
- Tracheo-innominate fistula
- Bleeding from an invading tumor
- DIC
- Infection
- Local irritation or erosion
- Must differentiate from bleeding from around the tracheostomy (i.e. superficial bleeding)
- All bleeding is highly concerning
- Diagnosis of cause
- Bronchoscopy, arteriography, and CT angiography can be helpful with diagnosis but have a low sensitivity (20% to 30%) (Sashida 2010)
- During the acute bleeding period direct visualization should occur in an OR setting and should not be delayed by diagnostic examinations.
- During the acute bleeding period, bronchoscopic examination is very difficult as the entire tracheal tree could be filled with blood (Yang 1988). Your ENT consultant may ask for imaging to help aid in diagnosis however this should occur on a case by case basis and only if the patient is stabilized.
-
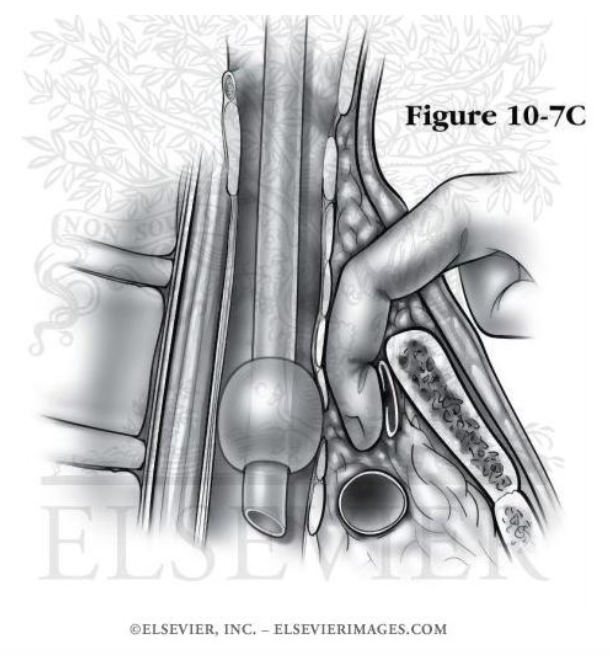
Tracheo-innominate Fistula Digital Compression (elsevierimages.com)
Management
- Call for surgical backup
- All bleeding should be considered dangerous regardless of volume or cessation and should be evaluated in an OR setting.
- You will have to manage and resuscitate the patient but ultimately they will need to go to the OR
- Over-inflate the cuff to tamponade bleeding (successful in 85% of cases of tracheoinnominate fistula) (Jones 1976)
- If Bleeding Continues
- Secure the airway with endotracheal intubation
- Remove the tracheostomy and insert a finger into the stoma to compress the innominate artery
- Digitally compress the innominate artery anteriorly
- Correct underlying any underlying coagulopathy and reverse anticoagulants
- If a central line is needed it can be placed in the right subclavian or a femoral vein. (Internal jugular venous access will obscure the operative field while left subclavian access may be rendered ineffective if the innominate vein is ligated) (Ailiwadi 2009)
- Call for surgical backup
- Infection management
- May present with bleeding, obstruction fever, cough, shortness of breath
- Infectious compications
- Cellulitis
- Tracheitis
- Mediastinitis
- Pneumonia
- All infectious complications should be treated with IV antibiotics
- Emergency Oxygenation
- If patient cannot ventilate after removal/attempted replacement or there is continued bleeding from stoma site need to use emergency oxygenation maneuvers
- Oral airway maneuvers (BVM, LMA) while covering stoma
- Stoma ventilation (pedi facemask or LMA to stoma) while occluding the nose and mouth
- If that fails attempt oral intubation using a long uncut tube to advance beyond the stoma or intubation of the stoma using a bougie or fiberoptic scope
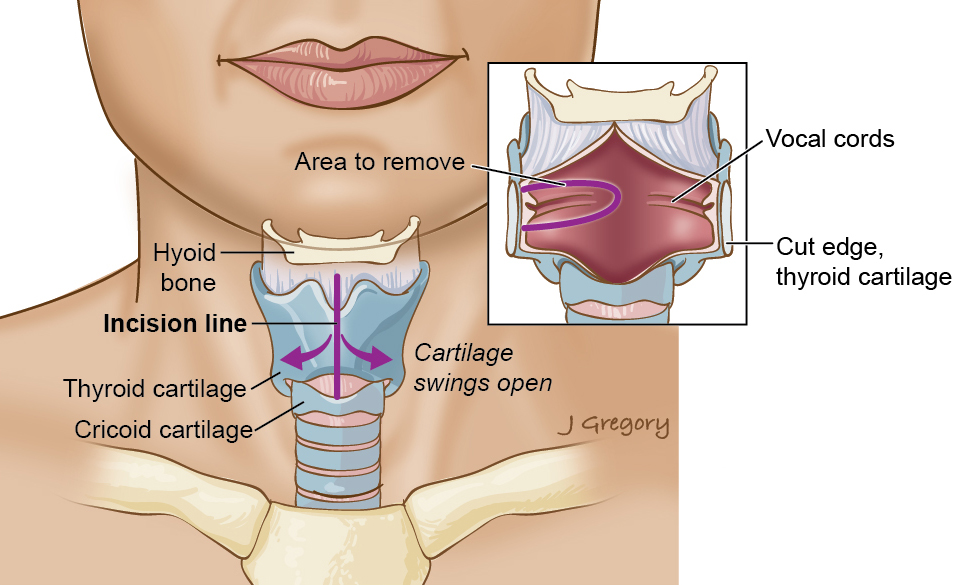
Laryngectomy Anatomy (headandneckcancerguide.org)
Laryngectomy Review (Mcgrath 2012)
- Typically due to a head and neck cancer
- Much less common than a tracheostomy
- There is NO PATENT UPPER AIRWAY
- May have a device like a TEP valve in situ- DO NOT REMOVE
- Exclusion of the upper airway means laryngectomy patients will not obstruct their airway when laying flat on their back and aspiration of gastric contents is not a concern. In the context of cardiopulmonary resuscitation, chest compressions will generate more significant tidal volumes owing to a reduction in dead space
Take Home Points
- The tracheostomy tract is considered mature after 7 days. Prior to this, blind replacement of the tracheostomy is discouraged
- Any bleeding from or around the tracheostomy should be considered due to a tracheo-innominate fistula and is a surgical emergency. All tracheostomy bleeding should be evaluated by a surgeon preferably in the OR
- If the patient cannot ventilate through the tracheostomy take it out and either replace it or intubate from above
References:
- Mcgrath BA et al. Guidelines Multidisciplinary guidelines for the management of tracheostomy and laryngectomy airway emergencies. N Anaesthesia 2012; 67 (9), 1025–1041. PMID: 22731935
- Engels P et al. Tracheostomy: from insertion to decannulation. Can J Surg. 2009 Oct; 52(5): 427–433. PMC: 2769112
- Grant C et. al. Tracheo-innominate artery fistula after percutaneous tracheostomy: three case reports and a clinical review. Br J Anes 2006; 96 (1): 127–31. PMID: 16299043
- GrilloCG: Tacheal fistula barchiocephalic artery, in GrilloCG (ed): Surgery of the Trachea and Bronchi. Hamilton, Ontario, BC Decker, Ch. 13, 2003, pp 1-9.
- Ailawadi G. Technique for Managing Tracheo-Innominate Artery Fistula.Operative Techniques in Thoracic and Cardiovascular Surgery. 2009; 14(1):66–72. Link
- Sashida Y et al. Successful management of tracheoinnominate artery fistula using a split pectoralis muscle flap with anatomical reconstruction by a synthetic graft. Scand J Plast Reconstr Surg Hand Surg 2010; 44 : 175-177.PMC: 20158425
- Yang FY, Criado E, Schwartz JA, Keagy BA, Wilcox BR : Trachea-innominate artery fistula : retrospective comparison of treatment methods. South Med J 81 : 701-706, 1988. PMID: 3287639
- Jones JW et al: Tracheo-innominate artery erosion: Successful surgical management of a devastating complication.Ann Surg. 1976;184:194-204. PMC: 1344431
- Seung WB et al. Successful Treatment of Tracheoinnominate Artery Fistula Following Tracheostomy in a Patient with Cerebrovascular Disease. J Korean Neurosurg Soc. 2012 Dec; 52(6): 547–550. PMID: 23346327