Originally published at CoreEM.net, dedicated to bringing Emergency Providers all things core content Emergency Medicine available to anyone, anywhere, anytime. Reposted with permission.
Follow Dr. Swaminathan and CORE EM on twitter at @EMSwami and @Core_EM
Written by: Anand Swaminathan, MD
Background
- Exists in two states
- Free ionized form (approx. 50%)
- Bound to other molecules (primarily albumin)
- Ionized Ca2+ concentration is inversely proportional to pH
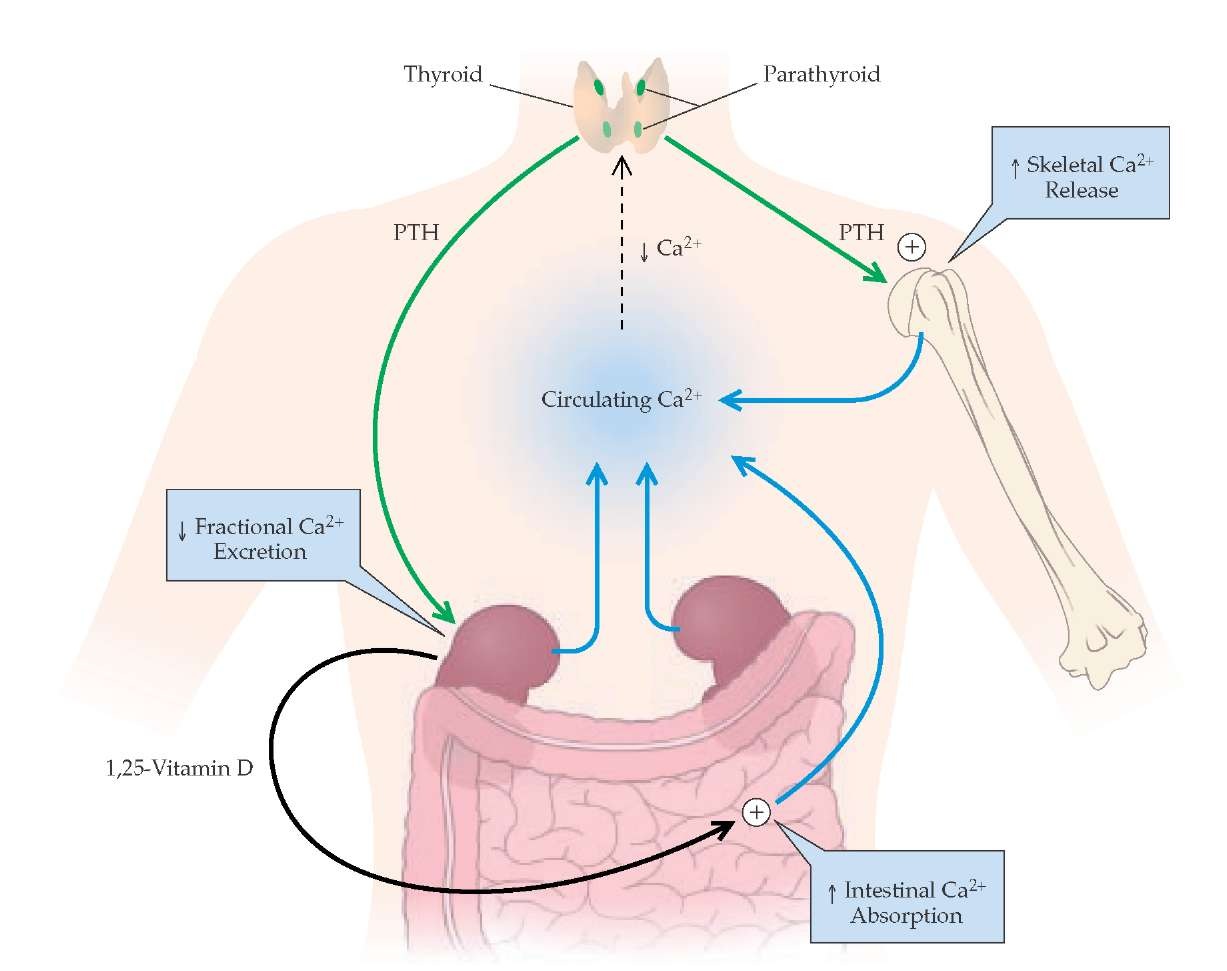
Calcium Metabolism – what-when-how.com
- Ca2+ Metabolism
- Vitamin D: aids in intestinal Ca2+absorption
- Parathyroid hormone (PTH)
- Increases renal Ca2+reabsorption
- Arbitrates Vit D stimulated intestinal Ca2+absorption
- Mobilizes Ca2+ from bone
- Calcitonin
- PTH antagonist
- Inhibits renal Ca2+ reabsorption
- Inhibits Ca2+ mobilization from bone
- Ca2+ plays numerous critical roles including muscle contraction (skeletal and smooth), clotting factor activity and nerve conduction
Causes
- Malignancy (multiple myeloma, metastases to bone)
- Granulomatous disease (TB, sarcoidosis)
- Endocrine (hyperthyroidism, hyperparathyroidism, adrenal insufficiency, pheochromocytoma)
- Pharmacologic agents (thiazide diuretics, milk-alkali syndrome, PTH therapy for osteoporosis, lithium, Vitamin A)
- Miscellaneous (Dehydration, rhabdomyolysis, prolonged immobilization, dietary, iatrogenic)
Clinical Manifestations
- “Stones (renal), Bones (bone pain), Groans (abdominal pain) + Moans (Psychiatric overtones)”
- Cardiac Effects
- Bradydysrhythmias
- AV block
- Sinus Arrest
- Atrial Fibrillation
- Ventricular Tachycardia
- QTc shortening
- Neuropsychiatric Disorders
- Major: AMS, seizures, weakness, lethargy, coma
- Minor: Anxiety, depression, confusion, hallucinations
- Hyporeflexia
Diagnosis
- Serum calcium > 10.5 mg/dL
- 5 – 12.0 mg/dL considered moderate
- > 14 mg/dL considered severe + potentially life-threatening
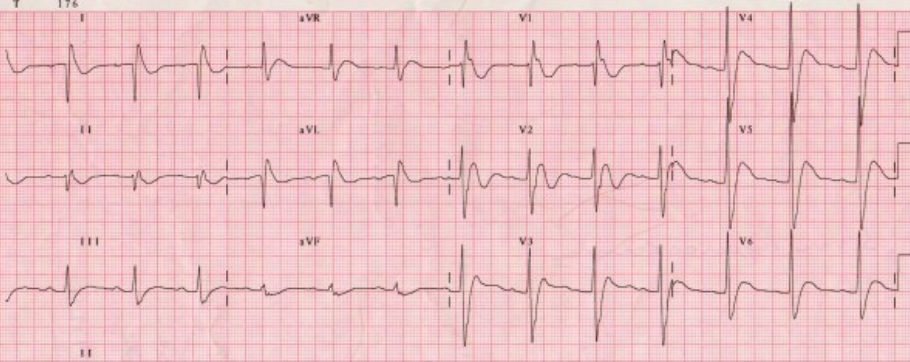
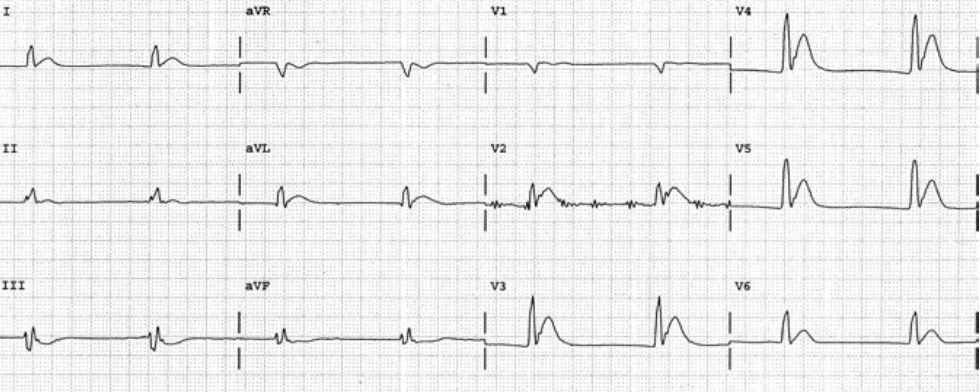
- EKG
- Short QTc interval (also caused by congenital short QT syndrome and digoxin)
- Prolonged PR
- Widened QRS complex
- AV block
Management
- Supportive Care – ABCs, IV, O2, Monitor
- Volume Expansion
- The majority of patients with hypercalcemia have significant dehydration
- Normal saline administration
- Mechanism of action: Corrects volume depleted state and inhibits proximal tubule calcium resorption
- Monitor other electrolytes (potassium, sodium)
- Dose
- Bolus to correct hypotension
- Careful administration while monitoring overall fluid status (patients often have cardiac and/or renal dysfunction making them susceptible to volume overload)
- Loop diuretics (i.e. furosemide)
- Mechanism of action: Inhibits reabsorption of Na,K, Cl via the Na+-K+-2Cl– cotransporter in the ascending loop of henle, thereby also inhibiting Ca2+ and Mg2+ reabsorption
- Theoretical benefit of “forced diuresis” not proven in the literature
- Should NOT be given until volume repletion completed as it can exacerbate hypercalcemia in this situation
- Bisphosphonates
- Mechanism of action: inhibit osteoclast-mediated bone resorption
- Zoledronic acid
- Preferred in hypercalcemia in the setting of malignancy
- Dose: 4 mg IV over 15 minutes
- Other Agents: Pamidronate, Etidronate
- Calcitonin
- Mechanism of action: inhibits Ca2+ absorption in the intestines, inhibits osteoclast activity, stimulates osteoblastic activity, inhibits renal tubular cell reabsorption
- Dose: 4 IU/kg IM Q12
- Cinacalcet
- Mechanism of action: increases the sensitivity of Ca2+ receptors on parathyroid cells to reduce PTH levels and, thus Ca2+ levels
- Indications: Hypercalcemia in patients with secondary hyperparathyroidism (i.e. CKD on dialysis, parathyroid carcinoma)
- Other
- Hemodialysis
- Parathyroidectomy may be considered in patients with hypercalcemia caused by hyperparathyroidism
Take Home Points
- Patients with severe hypercalcemia (> 14 mg/dL) are at risk for severe cardiac dysrhythmias and cardiac collapse
- Treatment centers on volume repletion with normal saline with consideration for the addition of loop diuretics AFTER volume reexpansion is complete
- As the patient begins to diurese, continually monitor electrolytes
References
Pfenning CL, Slovis CM: Electrolyte Disorders; in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2014, (Ch) 125: p 1636-53.
Read More
LITFL: QT Interval
LITFL: Hypercalcemia
LITFL: Hypercalcemia








1 thought on “CORE EM: Hypercalcemia”
Pingback: emDOCs.net – Emergency Medicine EducationMultiple Myeloma Emergencies - emDOCs.net - Emergency Medicine Education