Author: Jamie Santistevan, MD (@jamie_rae_EMdoc – EM Physician, Presbyterian Hospital, Albuquerque, NM) // Edited by: Manpreet Singh, MD (@MPrizzleER – Assistant Professor of Emergency Medicine / Department of Emergency Medicine – Harbor-UCLA Medical Center) and Brit Long (@long_brit – EM Attending Physician, San Antonio, TX)
Welcome to this edition of ECG Pointers, an EMDocs series designed to give you high yield tips about ECGs to keep your interpretation skills sharp. For a deeper dive on ECGs, we will include links to other great ECG FOAMed! This is part II of our AV blocks series, so please check out part I here.
The Case:
A 73-year-old woman presents with two days of fatigue and dyspnea on exertion. She is asymptomatic at rest and her BP is 165/90. Here is her ECG:

There is bradycardia with a ventricular escape rate of 39. At first glance it appears that there is a progressively lengthening PR interval. Looking closer at the rhythm strip you see some additional P-waves buried in the T-waves of the first two beats*.
The pacer pads are placed on her chest and this strip is recorded:
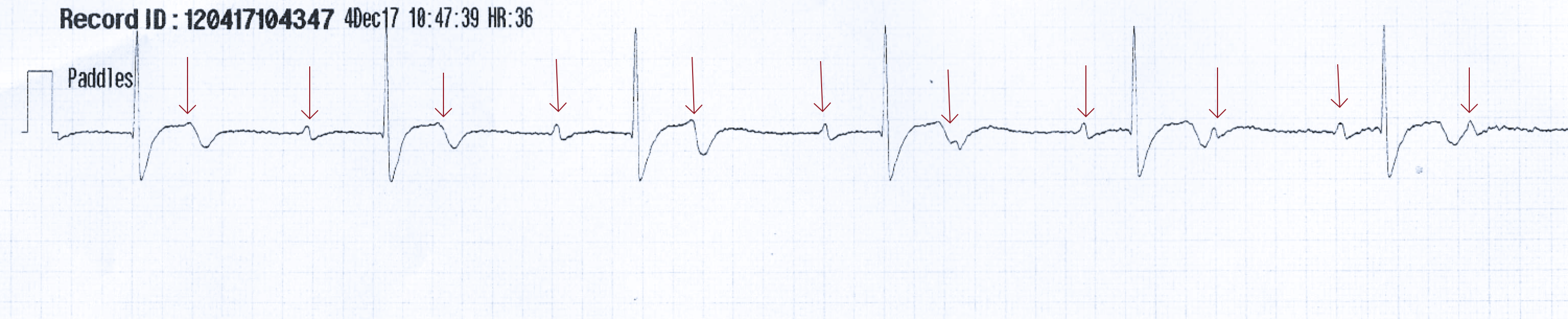
P-waves are marching at their own rate of about 65, the ventricles are conducting at 36 bpm. The QRS duration is prolonged.
Because she is asymptomatic at rest and hemodynamically stable, you do not externally pace her in the ED, but she is transferred urgently to the cath lab for a placement of a permanent pacemaker.
Mobitz II and complete AV block:
Second-degree Mobitz type II and third-degree (complete) AV block almost always results from conduction system failure below the level of the AV node. The ventricular rhythm is determined by either junctional or ventricular escape beats. In complete heart block there is no conduction through the AV node; the atria and ventricles are completely dissociated and there is no relationship between the two. The dissociation can produce severe bradycardia or even ventricular standstill and sudden cardiac death.
Reversible causes most commonly are myocardial infarction with ischemia of the AV node and medications (e.g. beta blockers, calcium channel blockers). Nonreversible causes included fibrosis of the conduction system (e.g. Levs disease), cardiac surgery, autoimmune conditions (e.g. SLE) and infiltrative myocardial disease (e.g. amyloidosis, hemochromatosis) [1].
For patients who are symptomatic or hemodynamically unstable, immediate treatment should be initiated to maintain perfusion. These patients may require pharmacologic intervention as a temporizing measure (chronotropic agents such as epinephrine). A trial of atropine as a temporizing measure may be used, but pacing is the definitive treatment. External pacing with transcutaneous pacer pads can be used while inserting a transvenous pacemaker with eventual placement of a permanent pacemaker by cardiology.
Second-degree Mobitz type II: what to look for on the ECG:
- There will be occasional non-conducted P-waves
- The PR interval will be constant for all conducted beats
- There is usually a fixed ratio of conduction between the atria to the ventricles (e.g. 3:2, 4:3).
- The QRS complex may be wide (about 75% of cases)
https://lifeinthefastlane.com/ecg-library/basics/mobitz-2/
Third-degree (complete) AV block: what to look for on the ECG:
- There is no association between the atria and ventricles (the PR interval is wildly inconsistent because of this)
- The atrial rate is usually normal 70-100 bpm
- The ventricular escape rate is usually 40-60 bpm
- The QRS duration is usually wide

https://lifeinthefastlane.com/ecg-library/basics/complete-heart-block/
How to differentiate Mobitz I and II:
In Mobitz I block, the AV nodal cells progressively fatigue and then fail producing lengthening PR intervals. In Mobitz II the conduction system suddenly fails to conduct a beat, leaving the PR interval constant prior to sudden failure.
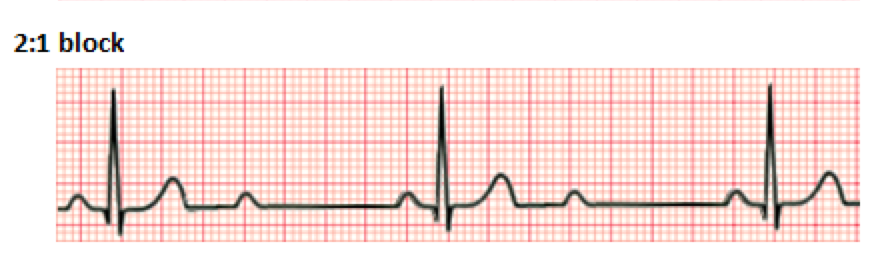
For patients with second degree AV block with a ratio of atrial to ventricular conduction of 2:1, the distinction between Mobitz type I and Mobitz type II cannot be made from the surface ECG alone.
https://en.wikipedia.org/wiki/Second-degree_atrioventricular_block
Other clues on the ECG may exist. In most cases of Mobitz I, the block occurs within the AV node and a junctional escape rhythm occurs with a rate between 40-60 bpm with a narrow QRS complex. When the block is below the AV node (Mobitz II and complete heart block), a ventricular escape rhythm produces a wide QRS complex with rates that are much slower (20-40 bpm) [2].
QRS complex duration and rate of ventricular conduction are not perfect clues because up to to one fourth of cases with Mobitz II may produce a junctional rhythm with a narrow QRS complex. Alternatively, Mobitz I may also occur in a patient with a pre-existing bundle branch block creating a wide QRS complex. The best way to know for certain is to observe patients for a period of time. A long rhythm strip should be recorded to watch for an occasional conduction pattern other than 2:1 (eg, 3:2, 4:3). A lengthening PR interval would suggest Mobitz type I (Wenckebach), and a consistent PR interval, Mobitz II.
Lastly, atropine could be administered to help distinguish the level of AV block. A lack of response to atropine is consistent with blockage occurring below the AV node and suggests Mobitz type II.
High-grade AV blocks:
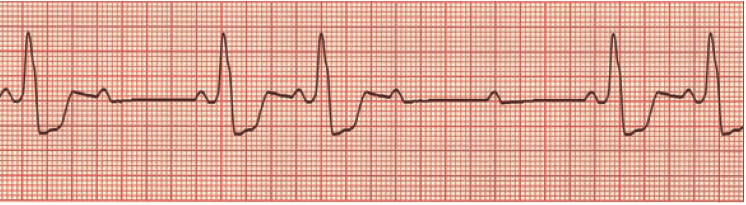
Mobitz I and Mobitz II can occasionally produce high-grade blocks, with rates of atrial to ventricular conduction greater than 2:1:

Atrial to ventricular conduction is 3:1. There is a wide QRS complex with a rate of 33 (ventricular escape). The PR interval is the same for each conducted beat (there is still a relationship between the atria and ventricles). It is impossible to determine if this is Mobitz I or Mobitz II second-degree block.
In cases of high-grade blocks, bradycardia is severe. Regardless of type of block (Mobitz I or II), these patients often need pharmacologic intervention and pacemaker placement.
The top ECG pointers for Mobitz II and Complete AV block:
- Mobitz II and complete AV block often occur due to blockade below the level of the AV node producing ventricular escape rhythms.
- Distinguishing between Mobitz I and Mobitz II is difficulty when there is 2:1 conduction and may require a prolonged rhythm strip, evaluation of QRS duration and PR intervals and a trial of atropine.
- High-grade second-degree blocks, Mobitz II and complete AV block require pacemaker placement.
But wait, there’s more ECG FOAMed:
- Practice your ECG interpretation skills for AV blocks at: http://www.tamingthesru.com/blog/diagnostics/back-on-the-block-heart-blocks-part-2
- For an interesting case of complete AV block caused by STEMI, look here: http://hqmeded-ecg.blogspot.com/2012/04/intermittent-third-degree-heart-block.html
- An in-depth analysis of an unusual rhythm caused by high grade AV block can be seen in this post: http://ecg-interpretation.blogspot.com/2017/12/ecg-blog-144-bradycardia-av-block_53.html
- Unstable and symptomatic bradycardias require urgent intervention. This is an overview of bradycardias and how to approach them in the emergency department: http://www.emdocs.net/approach-bradycardia-ed/
References:
- Sauer WH. Etiology of atrioventricular block. Nov 2017. Uptodate.com
- Yealy, D. M., Kosowsky, J. M. (2014). Dysrhythmias. In Rosen’s Emergency Medicine: Concepts and Clinical Practice 8th edition(pp. 1034-1046). Philadelphia, PA: Elsevier Saunders.







