Authors: Lloyd Tannenbaum, MD (EM Attending Physician, APD, Geisinger Wyoming Valley, PA) // Reviewer: Brit Long, MD (@long_brit)
Hello and welcome back to ECG Pointers, a series designed to make you more confident in your ECG interpretations. This week, we feature a post from Dr. Tannenbaum’s ECG Teaching Cases, a free ECG resource. Please check it out. Without further ado, let’s look at some ECGs!
“Wake up! No sleeping in Grand Rounds!” Your chief barks at you. “I don’t care if you’re coming off a night shift and are sleepy. Wake up and pay attention. AV Blocks will be on your in-training exam.”
Damn, you think to yourself. She caught me again. As you listed to the attending monotonously drone on about PR intervals, your eyes start to close and you drift back to a stressful night you had last month in the ER…
“…HEY INTERN! FOCUS!”
Another great shift with that jackass attending who refuses to learn any of the intern’s names. I love residency training, you think to yourself. “Sorry Sir! I’ll take a closer look at Mr. Deltar’s ECG.”

“Well.. Uh, Rate, rhythm, uhhh STEMI? Is that how I read them?” you ask, still not completely focused.
“Since you were daydreaming on shift again, let’s take this wonderful teaching opportunity to review AV blocks, Intern,” you staff gruffly tells you.
“I’d love nothing more, Sir!” you tell him, hoping he didn’t catch that it was dripping with sarcasm. He hands you this ECG to take a look:

“Well, Intern, don’t keep us waiting. Talk us through what you are seeing and remember to use the rate/rhythm/axis/intervals/morphology format that seemed to elude you earlier, he says with a sneer.
“Yes Sir!” You say, hoping that your voice isn’t trembling as much as your hands. I see:
Rate: 66 beats per minute
Rhythm: Well, there isn’t a 1:1 ratio of P:QRS, no NOT sinus rhythm
Axis: Normal
Intervals: There’s a dropped beat about 3 beats in, and then the PR interval gets progressively longer as the strip goes on
Morphology: Overall seems pretty reasonable, maybe some nonspecific ST-T changes
Final read: This ECG is consistent with a 2nd degree AV block type 1, also called a Mobitz 1 or Wenckebach AV block.
“Ok, better than expected, Mr. Bigshot. First, map out the PR intervals on the rhythm strip so I can double check you. And then, let’s see if you can go two for two…” and he hands you another ECG:
“Awesome, thank you for this learning opportunity…” Here’s the rhythm strip showing progressive PR prolongation:

“Notice that the PR interval gets (slightly) longer with each beat. Blue < Orange < Green < Yellow < Light Blue. And here’s my read of this next ECG:”

Rate: 75 beats per minute
Rhythm: Sinus rhythm
Axis: Left
Intervals: Prolonged PR interval (>200 msec or 1 big box)
Morphology: Pretty normal
Final Read: This ECG is consistent with sinus rhythm with a first degree AV block (Prolonged PR interval).
“Hmm. I thought that one was going to trip you up for sure. Maybe this one will” As he pulls yet another ECG from his pocket. “And don’t tell me it’s too wrinkled to read, you interns are such divas!” he grumbles at you.

Rate: 36 beats per minute
Rhythm: NOT sinus rhythm
Axis: Left
Interval: Narrow QRS complexes, no PR intervals, the P waves and the QRS complexes seem to be doing their own thing and not talking to each other.
Morphology: Some nonspecific ST-T wave changes
Final Read: The ECG is consistent with a third degree (complete) heart block. “Sir, I even included the rhythm strip that I marked up to show you what I’m seeing.”:
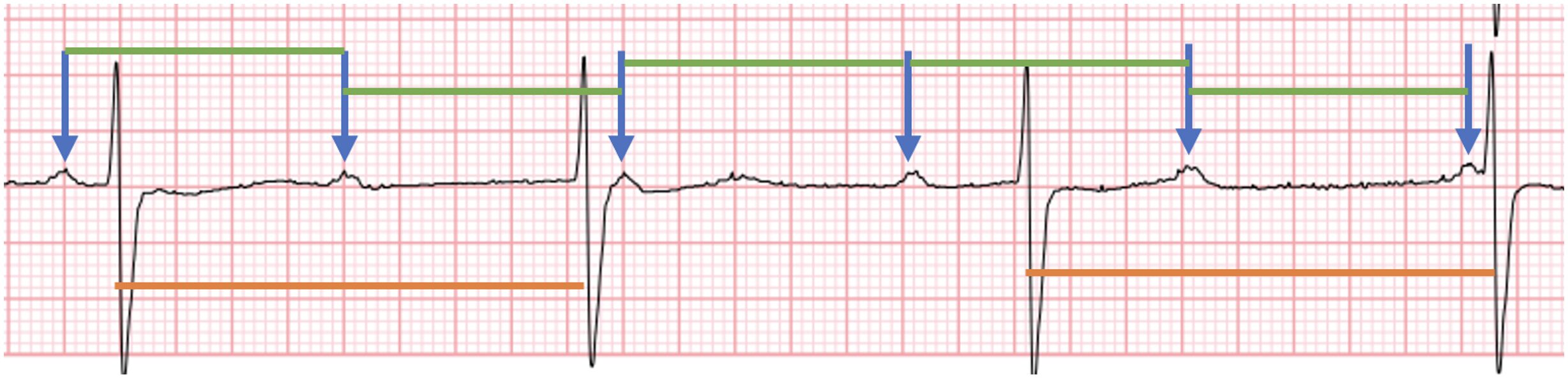
“Intern, looking at all your markings on that strip makes me want to vomit. Explain why you felt the need to draw a rainbow on my ECG!”
“Well Sir, the blue arrows show the P waves. All the green lines are the same and they show the P-P intervals. Notice how they march out evenly. Finally, the orange lines show the R-R intervals. They march out too and show that the P-P intervals (green) are different than the R-R intervals (orange), so the patient is in complete heart block.”
“Fine. 2 bonus points to you. Now that you’re awake and seem slightly more with it, take another look at Mr. Deltar’s ECG and take another shot at reading it. And while you’re at it, go ahead and color on my ECG to show me your point:
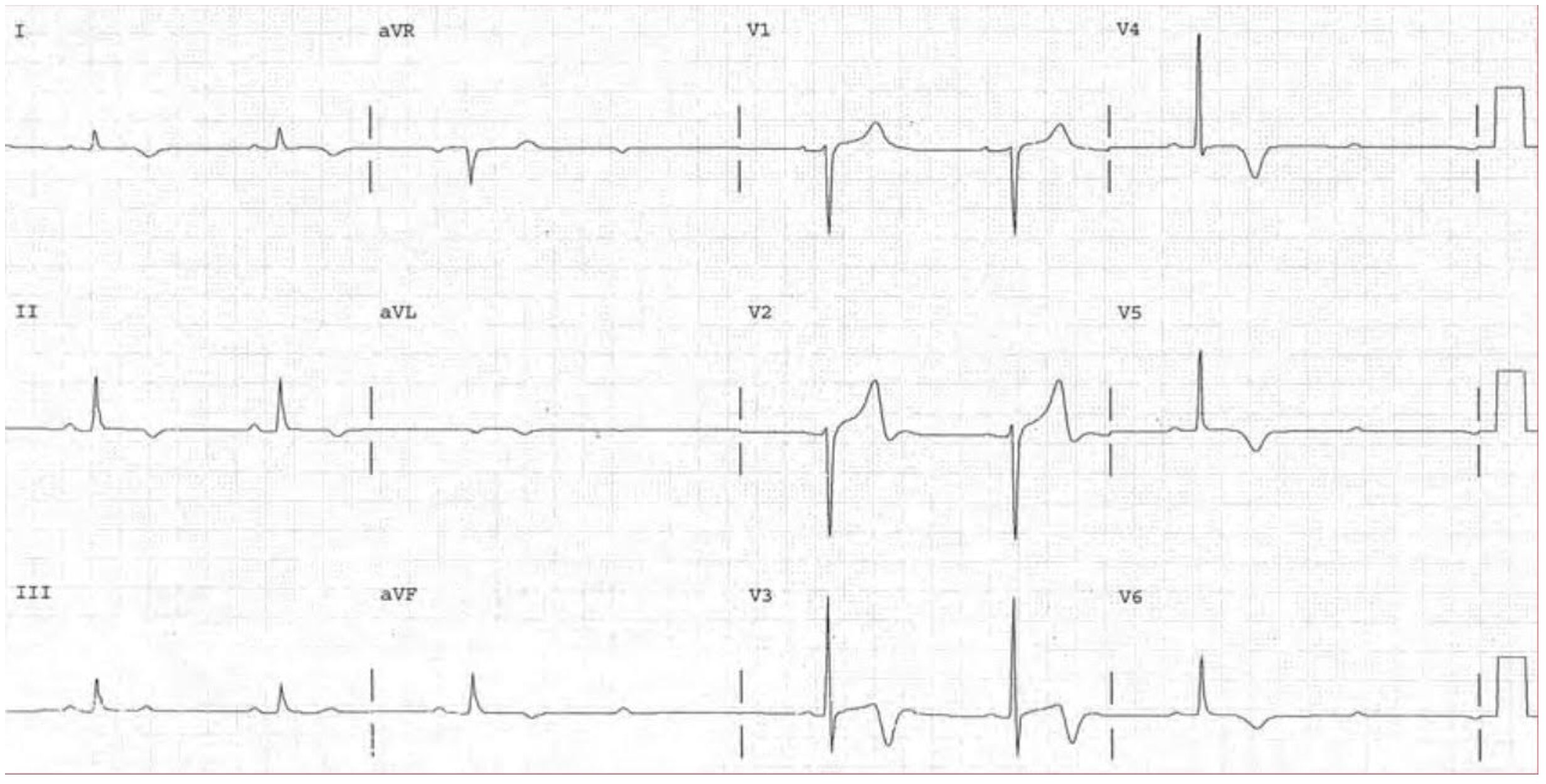
Rate: 36 beats per minute
Rhythm: NOT sinus. First of all, too bradycardic and second of all, not a 1:1 ratio of P:QRS complexes
Axis: Normal
Intervals: PR interval appears consistent between each beat, there is an occasional dropped beat
Morphology: Some nonspecific ST-T wave changes
Final read: This ECG is consistent with a second degree, Mobitz type 2 AV block. (Please note, it’s a touch tough to see here, since you’re looking at the PR interval across several different leads, but I’ll mark up a strip below to show the PR interval).
“Take a look at these strips I marked up, Sir! All the blue lines are the same length. It’s pretty consistent throughout. The PR interval on the one beat in aVF looks like it may be a touch longer than the preceding two, but other than that, they all look pretty consistent. I’d be concerned about a Mobitz 2 in this patient.”

“About time you figured out what’s going on with this patient. Now, Intern, explain to me why I care so much about Mr. Deltar’s ECG and why I can’t just send him home” your staff asks you.
“Well, sir, traditional teaching is that first degree AV block doesn’t cause much of a problem and these patients are usually totally fine. Second degree AV block comes in two different types. There’s Mobitz Type 1, which is also known as Wenckebach. In this process, the PR interval gets progressively longer and longer until there is a dropped beat. This one also doesn’t usually cause a problem and these patients are often safely discharged home. Then there’s Mobitz type 2, where the PR intervals are always the same interval and the beats drop randomly. This is the “bad” kind of Mobitz and needs to be discussed emergently with cardiology, as these patients will often degrade into 3rd degree AV block and will need a pacemaker. Finally, there’s third degree AV block, or complete heart block. This is where the atria and the ventricles are completely dissociated and march out independently. These patients need a pacemaker and emergent cardiology or electrophysiology consults.”
“Well, Intern, that was at least ok. But while you were yapping on, something’s gone wrong with Mr. Deltar. Go take a look at him. And do me a favor while you’re over there, do your best not to kill my patient.”
As you hustle over to check on Mr. Deltar, the nurse meets you in the room and hands you his telemetry strip:

“Oh! this is not good,” you tell your nurse. “Get the crash cart in here immediately! You can see Mr. Deltar convert from a 2:1 AV block into a 3rd degree AV block. He needs a pacemaker immediately!”
You check on your patient and find him very lethargic and in and out of consciousness. His blood pressure is in the low 80s systolic. You start transcutaneous pacing him which he describes as “ridiculously uncomfortable,” “horrendously uncomfortable” and “Freaking stop this right now.” Glad he’s tolerating pacing so well. You explain to the patient that you need to place a transvenous pacer to keep his heart beating and he tells you, “If it will let you stop shocking my chest every few seconds you can do anything you want.” You place a right IJ central line and float the pacer through it. You’re able to stop transcutaneous pacing Mr. Deltar, which he appreciates. The electrophysiology team is standing by to take the patient to the EP lab to place a permanent pacemaker.
“Well, Intern, you did a really nice job today, I’m proud of you” your staff tells you.
You turn around, shocked to hear him say something so positive, but he’s already gone down the hall to the next patient. He sees you looking at him and gives you a “Hurry up” gesture with a disappointed head shake. Moment over.
Let’s take a few seconds to recap AV blocks before we wrap up:
- First degree AV block just means that the PR interval is over 200 msec (one big box). It’s rarely cause for concern.
- Second degree AV blocks come in two different flavors.
- Type 1 (also known as a Mobitz 1 or Wenckebach) shows a progressive prolongation of the PR interval before the beat drops.
- This type of AV block is usually stable and doesn’t often cause trouble.
- Type 2 (also known as a Mobitz 2) keeps a preserved (unchanging) PR interval and then a beat just drops out of nowhere.
- This one is the troublemaker of the two. You can degrade into 3rd degree very easily. These patients are often taken for permanent pacemaker placement and need a stat cardiology consult.
- Type 1 (also known as a Mobitz 1 or Wenckebach) shows a progressive prolongation of the PR interval before the beat drops.
- Third degree AV block (also called complete heart block) shows no association between the P waves and the QRS complexes.







