Authors: Jose Gomez, MD (EM Resident Physician, UTSW – Dallas, TX); Jenna Bryant, MD, CAQSM (Assistant Professor of EM / Attending Physician, UTSW- Dallas, TX) // Reviewed by: Sophia Görgens, MD (EM Physician, Northwell, NY); Cassandra Mackey, MD (Assistant Professor of Emergency Medicine, UMass Chan Medical School); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
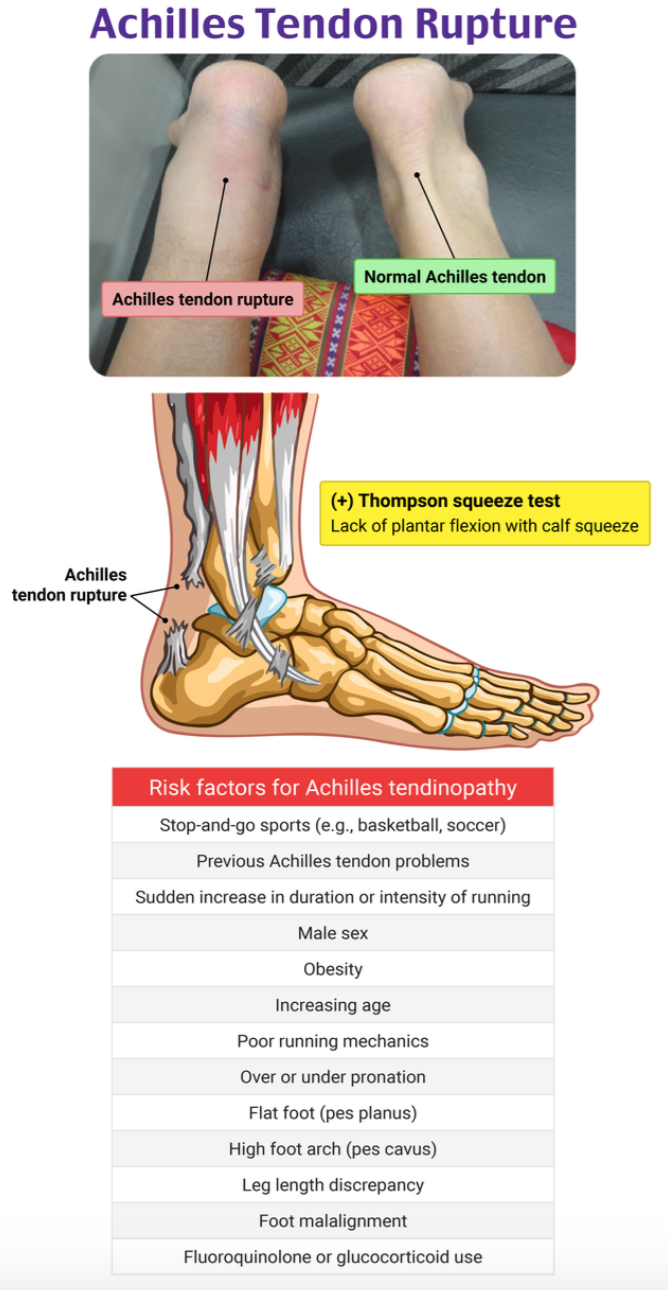
A 45-year-old man with no past medical history presents to the ED with right calf pain after playing basketball earlier today. As he began to run for a ball, he felt a sudden sharp pain in the back of his leg, as if he had been kicked. He can bear weight but is unable to push off with his right leg. On exam, there is swelling and tenderness on the posterior heel, but no ecchymoses or open wounds. He has full active flexion and extension in his right knee. Compartments are soft, and distal pulses are +2. Sensation is intact throughout the extremity. Ankle dorsiflexion is 4/5 and plantar flexion 0/5 on the right. Thompson test is positive.
Question: What is the diagnosis?
Answer: Achilles tendon rupture (ATR)
Epidemiology
- Incidence as high as 40:100,000 per patient population annually1
- Most commonly occurs during sports/exercise related activities (81.9%) and in those who are 20-39 years old (54.4%)2,3
- Higher occurrence in males versus females (77.1% vs 22.9%), men playing basketball (42.6%), women playing volleyball (15.2%)2
Background
- Achilles tendon is the largest and strongest tendon in the body4
- Ruptures usually occur 2-6cm above the calcaneal insertion site due to poor perfusion in this area5
- Ruptures range from partial thickness to complete thickness tears
- Partial tears are less common and often misdiagnosed as Achilles tendinopathy (pain, inflammation and stiffness of the tendon)6,7
- ATR caused by sudden plantar flexion, direct trauma, previous tendinopathy, sudden or violent dorsiflexion of foot9.10
- Risk factors:11,12
- poor conditioning/weekend warrior (person who participates in sports/hobbies only on weekends or leisure time)
- BMI > 25
- steroid injections
- fluoroquinolone antibiotics (disturbs interaction between cells and matrix by chelating divalent ions)13
- Achilles tendinopathy
- diabetes mellitus (increases intracellular content of water and increases cross-linking within collagen fibers due to glycosylation end-products)14
- parathyroid disorder (PTH affects bone resorption and remodeling, which can lead to ligament and tendon tissue degeneration)15
- SLE
- rheumatoid arthritis
- poor calf flexibility
- poor ankle dorsiflexion
- high-arched foot
- tibia vara
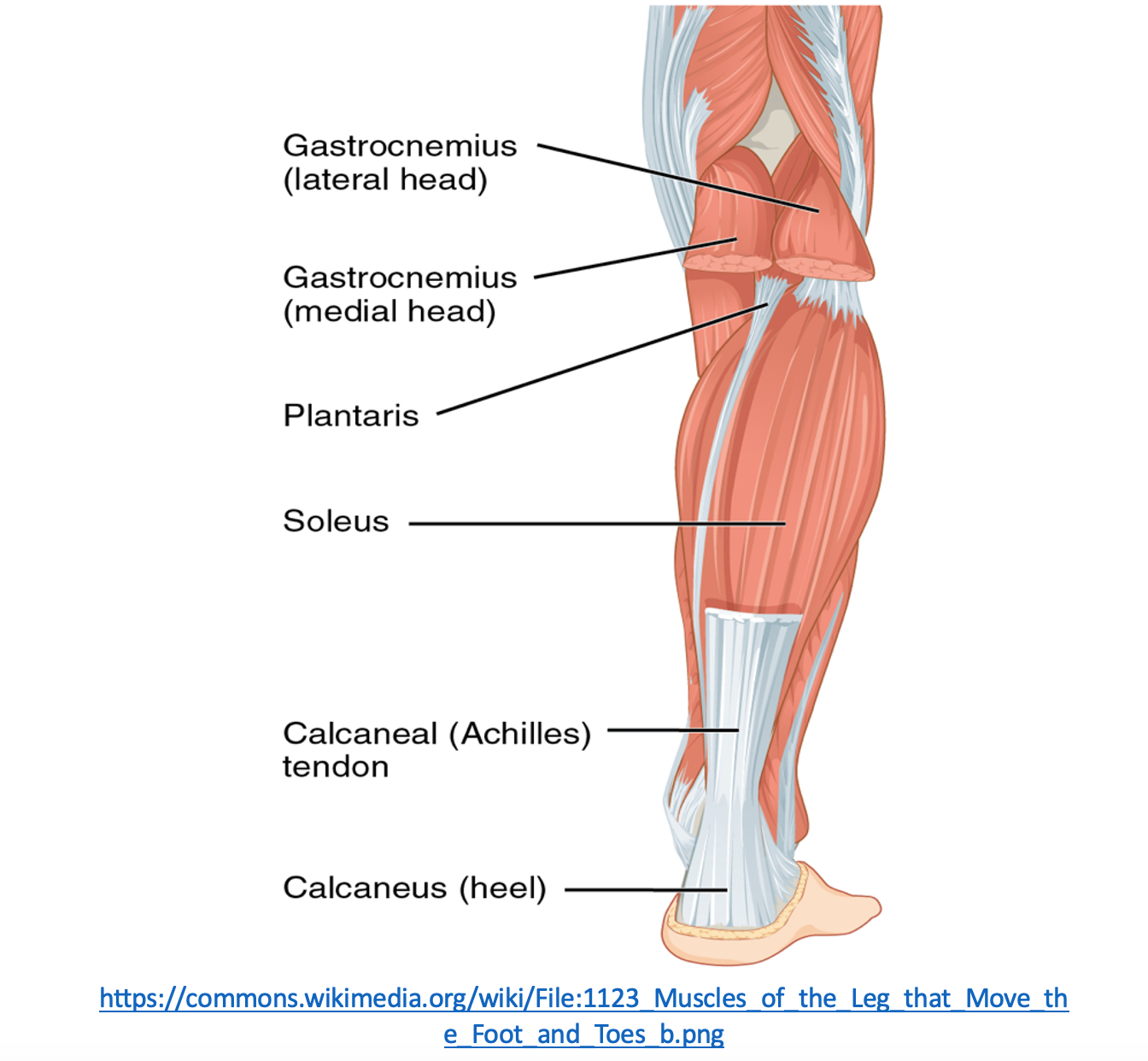
Anatomy
- Achilles tendon: formed by the confluence of the gastrocnemius, soleus, and plantaris muscles4
- Insertion: posterior surface of calcaneus
- Function: foot plantar flexion
- Innervation: sural nerve
- Blood supply: posterior tibial artery (proximal and distal), peroneal artery (middle)
Clinical Presentation
- Sudden onset of pain often described as being kicked in the lower leg
- Can be associated with an audible “snap” or “pop”
- Difficulty walking on affected leg due to inability to plantar flex foot8
Evaluation
- Obtain history on mechanism of injury, timing, other injuries, social and medical history, competitive athlete vs non athlete11
- Physical exam:
- Edema and ecchymosis may be present on the posterior calf
- Achilles palpation test: directly palpate the Achilles tendon and evaluate for any depression, gap, sulcus, or edema8,9
- Matles Test: Increased resting ankle dorsiflexion with knees bent at 90° in prone position8,9
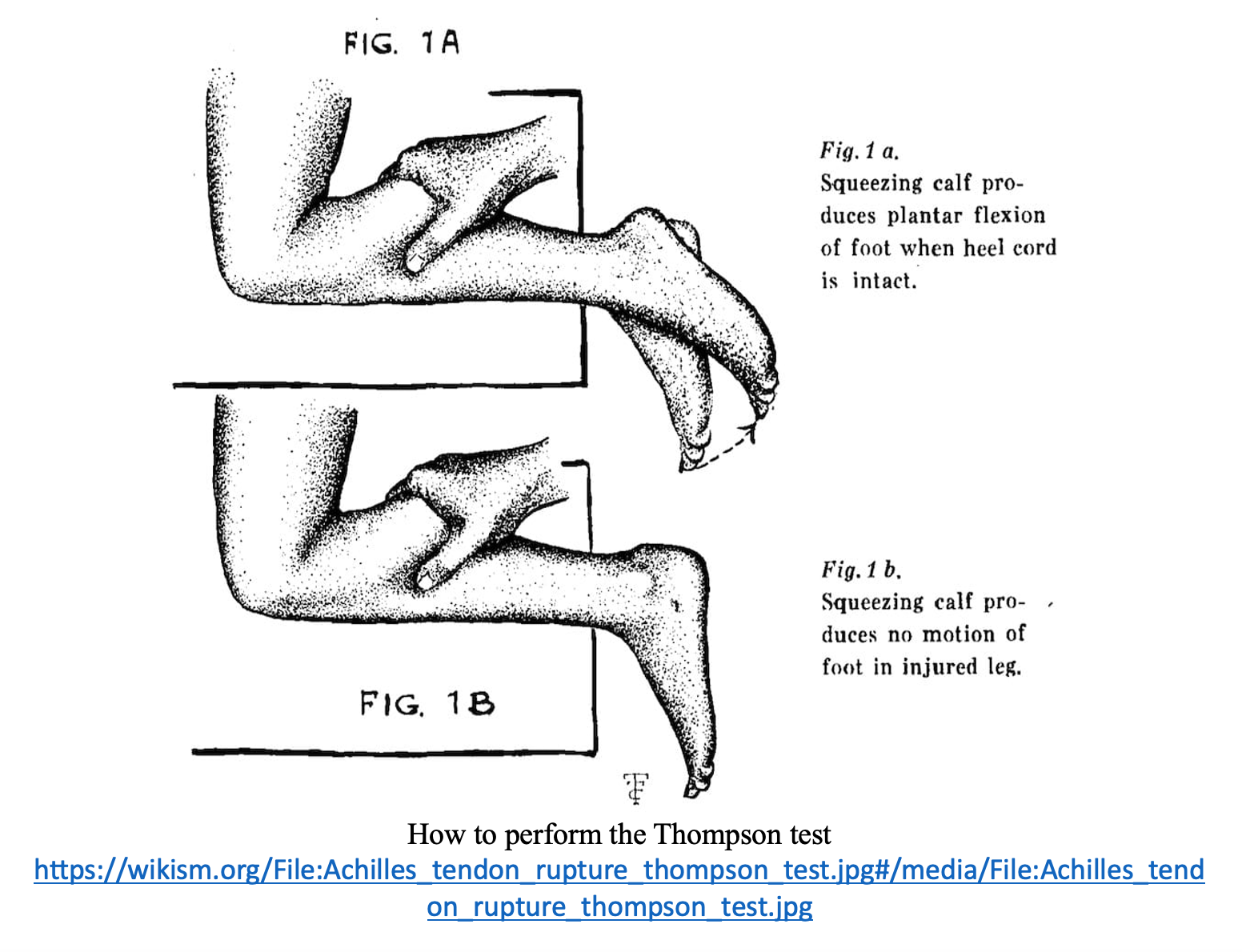
- Thompson test: lay patient prone with knee bent at 90° then squeeze the calf, perform on both legs; sensitivity 96% and specificity 93%8,9,16
- Normal: ankle plantarflexion
- Abnormal: no ankle plantarflexion (ATR), diminished plantarflexion with pain (partial ATR)6

Diagnosis
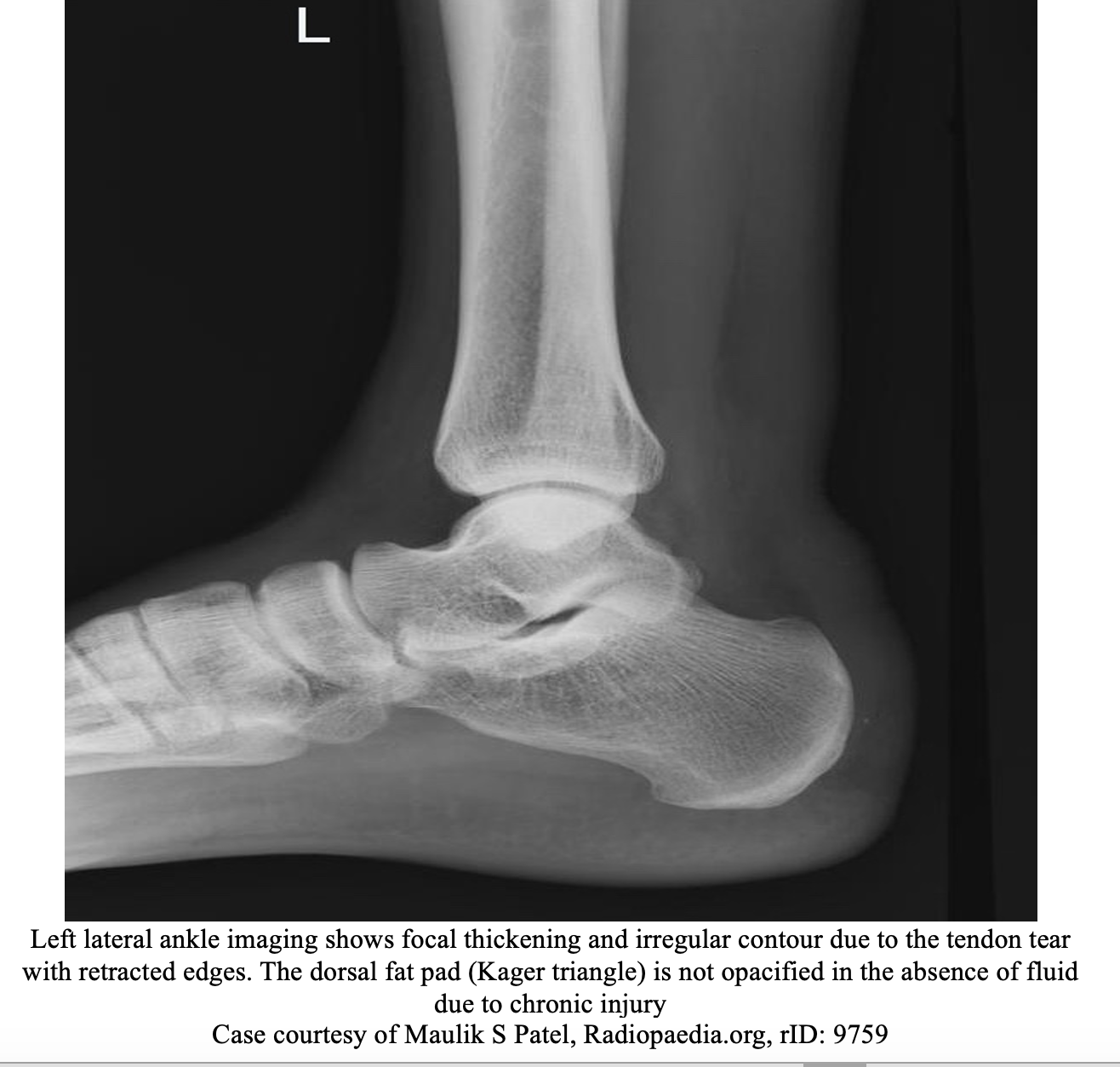
- Diagnosis typically made clinically, but imaging often ordered to rule out other injuries, confirm ATR, or for surgical planning11
- Ankle Xray: AP, lateral, mortise
- Tendon can demonstrate thickening and irregular contour17
- Pre-Achilles/Kager’s fat pad may be swollen or obliterated17
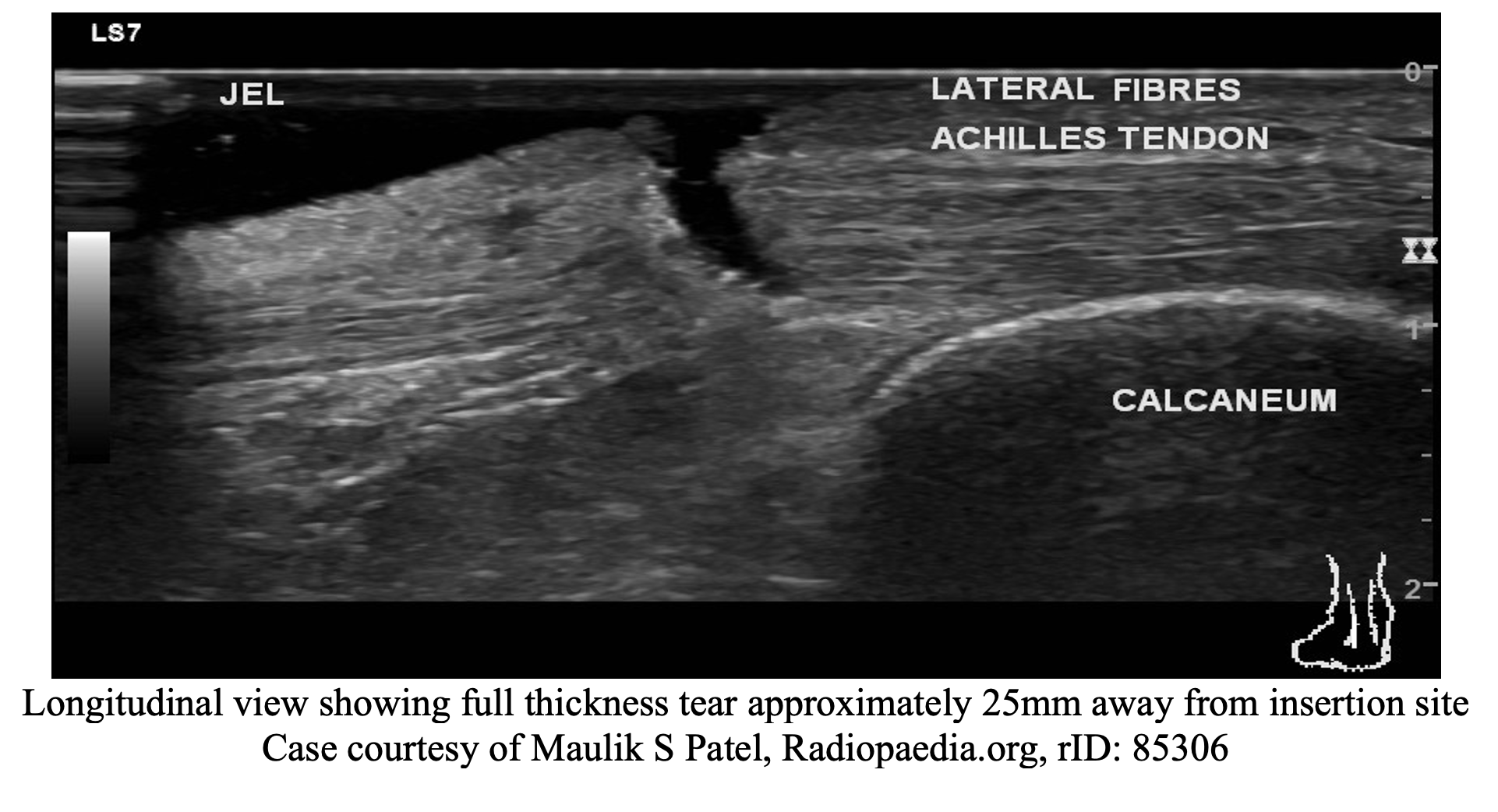
- Ultrasound (US): can help identify ATR vs partial ATR, sensitivity of 79-100%18
- Partial thickness tear: tendon thickening with bulging, wavy/irregular contour changes, focal hypoechoic or anechoic areas, increased blood flow on doppler6
- Full thickness tear: retracted tendon with contour changes; acoustic shadowing at the tear margins with adjacent hypoechoic tendinosis16
- Video on how to perform US
- MRI: obtained in ambiguous presentations and for preoperative planning11
- Superior to US in detection of partial tears19
Treatment/Management
- Non-weight bearing status until evaluated by orthopedics and physical therapy11
- ATR
- Non-surgical: Plaster cast vs functional brace
- Cast: AO splint (posterior short leg with stirrup) with ankle in 20-30° plantar flexion for 4-6 weeks8,9
- Brace: CAM/walking boot with 3-inch heel lift8,9
- Casting is not superior to functional brace in treatment20
- Can start early ROM after 3 weeks of immobilization as it does not lead to higher re-rupture vs no immobilization21
- Surgical Indications:
- Acute injuries (injury <6 weeks)
- Open wounds
- Failed conservative treatment for partial ATR
- High performance athletes
- Surgeon preference8,9
- Non-surgical: Plaster cast vs functional brace
- Partial ATR
- Non-surgical: no formal standardized evidence-based approach available6
- Brace vs cast and follow up with orthopedics
- Exercise based protocols based on case series and reports22,23
- Extracorporeal shock wave therapy, platelet rich plasma injections are possible adjunct treatments24,25
- Surgical: failed conservative management, high performance athlete
- Follow up with orthopedics
- Non-surgical: no formal standardized evidence-based approach available6
Disposition
- If open wounds or other fractures, consultation with orthopedics in the ED
- Outpatient referral to orthopedics and/or physical therapy
Pearls
- Achilles tendon rupture tend to occur more frequently in males and those who were engaged in a physical activity during the incident
- Diagnosis can me made clinically with history and exam (Thompson test), but imaging, such as x-rays and ultrasound can help rule out other injuries and differentiate partial versus complete tears
- Treatment involves casting in plantar flexion or a walking boot with a heel lift
- Close follow-up with orthopedics outpatient

A 36-year-old man presents to the emergency department with ankle pain. He states that he was jumping to grab a ball when he was playing basketball and felt a “pop” at the back of his ankle. On exam, he has a positive Thompson test. What is the most appropriate next step in care?
A) Apply a splint with the ankle in slight plantarflexion
B) Consult orthopedics for surgical evaluation
C) Obtain CT angiography of the extremity to rule out vascular compromise
D) Place the patient in a controlled ankle movement boot
Answer: A
This patient is presenting with an Achilles tendon rupture. These usually occur when sudden forces are exerted on the Achilles tendon. They often occur during strenuous activities that involve rapid acceleration or pivoting on a foot. Many patients will report feeling a pop or feel like they were struck at the back of their ankle. Patients often present with significant pain, and a defect is often easily identified and palpated. However, a small percentage of patients may present without pain or significant difficulty ambulating. Certain tests, such as the Thompson test, can help provide a more accurate means for diagnosing Achilles tendon ruptures on exam.
For this test, the patient lies prone with their knee flexed at 90°. The examiner squeezes the patient’s calf muscles which should cause contraction of an intact Achilles tendon, leading to plantar flexion. If the tendon is completely ruptured, no plantar flexion would be seen, leading to a positive finding. MRI may help differentiate the extent of the tear and could potentially differentiate between partial and complete tears, but this can be performed in the outpatient setting.
Initial care of Achilles tendon ruptures consists of conservative management, analgesics (anti-inflammatories), and immobilization with the ankle in slight plantarflexion. All patients should be discharged with close follow-up with orthopedic surgery, as many of these patients will be treated operatively.
Consulting orthopedic surgery in the emergency department (B) would be inappropriate, as an isolated Achilles tendon rupture is not an indication for emergency surgery.
Obtaining CT angiography of the extremity to rule out vascular compromise (C) is also inappropriate, as most Achilles tendon injuries caused by running and jumping are not significant enough to lead to vascular injury. Assessment for such should start with a physical exam, not imaging.
Placing the patient in a controlled ankle movement boot (D) would still allow some movement in the ankle. These patients should be immobilized in slight plantarflexion and placed in non-weight-bearing status when discharged from the emergency department.
Further Reading:
Further FOAMed
- https://www.emdocs.net/ultrasound-for-achilles-tendon-rupture/
- https://www.aliem.com/splinter-series-my-foot-doesnt-work-right/
References
- Meulenkamp B, Stacey D, Fergusson D, Hutton B, Mlis RS, Graham ID. Protocol for treatment of Achilles tendon ruptures; a systematic review with network meta-analysis. Syst Rev. 2018;7(1):247. Published 2018 Dec 23. doi:10.1186/s13643-018-0912-5
- Lemme NJ, Li NY, DeFroda SF, Kleiner J, Owens BD. Epidemiology of Achilles Tendon Ruptures in the United States: Athletic and Nonathletic Injuries From 2012 to 2016. Orthop J Sports Med. 2018;6(11):2325967118808238. Published 2018 Nov 26. doi:10.1177/2325967118808238
- Maffulli N, Via AG, Oliva F. Chronic Achilles Tendon Rupture. Open Orthop J. 2017;11:660-669. Published 2017 Jul 31. doi:10.2174/1874325001711010660
- Wong M, Jardaly AH, Kiel J. Anatomy, Bony Pelvis and Lower Limb: Achilles Tendon. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 8, 2023.
- Cao S, Teng Z, Wang C, Zhou Q, Wang X, Ma X. Influence of Achilles tendon rupture site on surgical repair outcomes. J Orthop Surg (Hong Kong). 2021;29(1):23094990211007616. doi:10.1177/23094990211007616
- Gatz M, Spang C, Alfredson H. Partial Achilles Tendon Rupture-A Neglected Entity: A Narrative Literature Review on Diagnostics and Treatment Options. J Clin Med. 2020;9(10):3380. Published 2020 Oct 21. doi:10.3390/jcm9103380
- Medina Pabón MA, Naqvi U. Achilles Tendinopathy. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 17, 2023.
- Karadsheh M MD. Achilles tendon rupture – foot & ankle – Orthobullets. https://www.orthobullets.com/foot-and-ankle/7021/achilles-tendon-rupture
- Achilles tendon rupture – WikiSM (Sports Medicine Wiki). WikiSM. Published December 10, 2023. https://wikism.org/Achilles_Tendon_Rupture#
- Tarantino D, Palermi S, Sirico F, Corrado B. Achilles Tendon Rupture: Mechanisms of Injury, Principles of Rehabilitation and Return to Play. J Funct Morphol Kinesiol. 2020;5(4):95. Published 2020 Dec 17. doi:10.3390/jfmk5040095
- Shamrock AG, Dreyer MA, Varacallo M. Achilles Tendon Rupture. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 17, 2023.
- Xergia SA, Tsarbou C, Liveris NI, Hadjithoma Μ, Tzanetakou IP. Risk factors for Achilles tendon rupture: an updated systematic review. Phys Sportsmed. 2023;51(6):506-516. doi:10.1080/00913847.2022.2085505
- Claessen FM, de Vos RJ, Reijman M, Meuffels DE. Predictors of primary Achilles tendon ruptures. Sports Med. 2014;44(9):1241-1259. doi:10.1007/s40279-014-0200-z
- Tarantino D, Mottola R, Resta G, et al. Achilles Tendinopathy Pathogenesis and Management: A Narrative Review. Int J Environ Res Public Health. 2023;20(17):6681. Published 2023 Aug 30. doi:10.3390/ijerph20176681
- Tao Z, Liu W, Ma W, Luo P, Zhi S, Zhou R. A simultaneous bilateral quadriceps and patellar tendons rupture in patients with chronic kidney disease undergoing long-term hemodialysis: a case report. BMC Musculoskelet Disord. 2020;21(1):179. Published 2020 Mar 19. doi:10.1186/s12891-020-03204-6
- Reiman M, Burgi C, Strube E, et al. The utility of clinical measures for the diagnosis of achilles tendon injuries: a systematic review with meta-analysis. J Athl Train. 2014;49(6):820-829. doi:10.4085/1062-6050-49.3.36
- Bell D, Gaillard F. Achilles tendon tear. Radiopaedia.org. Published online May 2, 2008. doi:53347/rid-836
- Dams OC, Reininga IHF, Gielen JL, van den Akker-Scheek I, Zwerver J. Imaging modalities in the diagnosis and monitoring of Achilles tendon ruptures: A systematic review. Injury. 2017;48(11):2383-2399. doi:10.1016/j.injury.2017.09.013
- Szaro P, Nilsson-Helander K, Carmont M. MRI of the Achilles tendon-A comprehensive pictorial review. Part one. Eur J Radiol Open. 2021;8:100342. Published 2021 Mar 26. doi:10.1016/j.ejro.2021.100342
- Costa ML, Achten J, Marian IR, et al. Plaster cast versus functional brace for non-surgical treatment of Achilles tendon rupture (UKSTAR): a multicentre randomised controlled trial and economic evaluation. Lancet. 2020;395(10222):441-448. doi:10.1016/S0140-6736(19)32942-3
- Barfod KW, Hansen MS, Hölmich P, Kristensen MT, Troelsen A. Efficacy of early controlled motion of the ankle compared with immobilisation in non-operative treatment of patients with an acute Achilles tendon rupture: an assessor-blinded, randomised controlled trial. Br J Sports Med. 2020;54(12):719-724. doi:10.1136/bjsports-2019-100709
- Masci L., Alfredson H. Promising results using a simple rehabilitation program to treat partial ruptures in the Achilles midportion. Biomed. Graph. Comput. 2013;3:47. doi: 10.5430/jbgc.v3n4p47.
- Medeiros DM. Conservative treatment of Achilles tendon partial tear in a futsal player: A case report. Physiother Theory Pract. 2021;37(10):1158-1165. doi:10.1080/09593985.2019.1683924
- Hsu Y.C., Wu W.T., Chang K.V., Han D.S., Chou L.W. Healing of Achilles tendon partial tear following focused shockwave: A case report and literature review. Pain Res. 2017;10:1201–1206. doi: 10.2147/JPR.S132951.
- Filardo G., Presti M.L., Kon E., Marcacci M. Nonoperative biological treatment approach for partial Achilles tendon lesion. 2010;33:120–123. doi: 10.3928/01477447-20100104-31.






