Author: Alessandra Della Porta, MD (@MedEdtweeter, EM Resident Physician, University of Cincinnati, Cincinnati, OH) // Reviewed by: Sophia Görgens, MD (EM Physician, Northwell, NY); Cassandra Mackey, MD (Assistant Professor of Emergency Medicine, UMass Chan Medical School); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
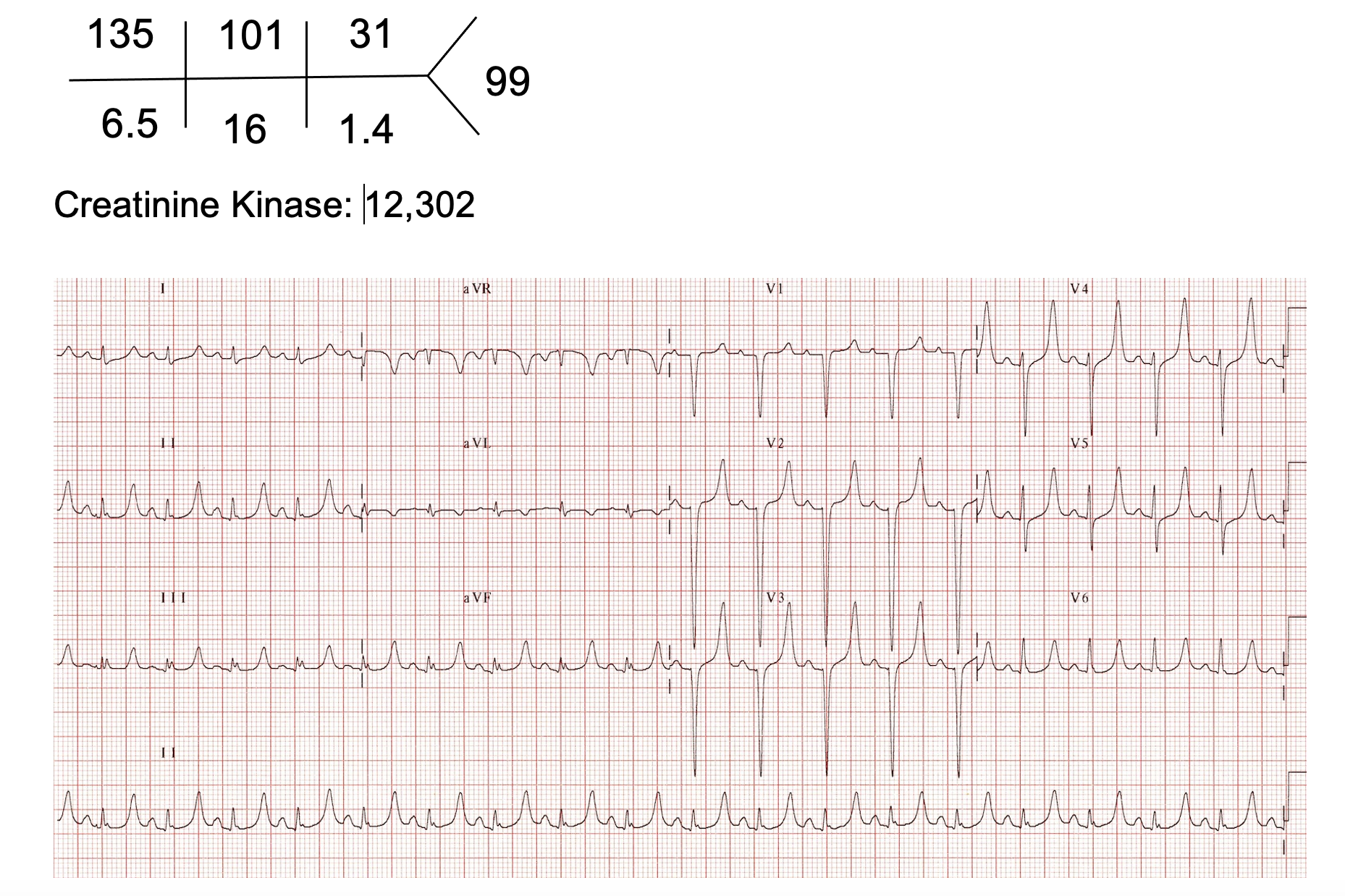
A 17-year-old girl, in moderate distress, is brought in by EMS after a motor vehicle collision. EMS reports that she was “pinned” underneath the dashboard, and it took several hours to extricate her. Triage vital signs significant for BP 103/69, HR 99, SpO2 99% on 2 L NC, RR 25, Temp 98.6. She has normal mental status but is in distress with severe pain in her legs. On exam she has erythema, ecchymosis, and gross deformities to bilateral lower extremities but intact distal sensation and palpable pulses. She refuses to move her legs secondary to pain.
Evaluation:
What is the cause of her hyperkalemia and the underlying diagnosis?
Answer: Crush injury resulting in release of intracellular potassium from damaged myocytes.
Introduction
- Crush injury: result of physical trauma from prolonged compression that initially causes direct tissue damage and later results in downstream effects from hypoxic conditions suffered by those tissues.1-3
- Common causes:
- Natural disasters such as tornadoes or earthquakes4,5
- Structure or building collapses from home fires or bombings.6
- Motor vehicle collisions that produce significant challenges to passenger extrication.6
- Prolonged down time from falls, usually in the elderly
- Incidence is difficult to ascertain due to broad definition and that events that cause crush injuries are rather rare.
- The incidence of a similar condition, traumatic rhabdomyolysis, is estimated to be around 0.074%.7
- 74% of crush injuries occur to the lower extremities8
- Risk factors9
- Male Sex
- Age < 35 years
- BMI >40
Pathophysiology
- Morbidity = Force x Duration
- Mechanisms of tissue damage
- Direct: fractures, vascular injuries, and shearing force on muscle fibers
- Ischemic: Impairment of arterial and venous flow leading to ischemia and anaerobic metabolism1
- Reperfusion: Blood containing reactive oxygen species returns to limb, while high acidic blood containing myoglobin and toxic concentrations of electrolytes enters the systemic circulation10,11
Clinical Presentation
- Crush injuries rarely present a diagnostic dilemma, given that the patient or EMS personnel transporting the patient for care will provide a history of recent trauma
- Classic Triad: dark urine, myalgias, weakness12,13
- Present < 10 % patients
- Most common symptom is myalgias (84% of patients)14
- Common associated injuries include pelvic or long bone fractures, intrathoracic or intra-abdominal injuries, including asyphxiation15
- Examination
- Musculoskeletal: Evidence of fracture, pain with palpation
- Dermatologic: Spectrum from erythema => ecchymosis => purpura => mottling
Evaluation
- ABCs: Treat these as trauma patients first and manage according to ATLS guidelines
- Objective findings
- Dehydration, hemorrhage, third spacing => hypotension10
- Malperfusion and myoglobin cytotoxicity => renal failure and kidney injury11,16
- Damaged myocytes => electrolyte derangements8
- Ischemia => lactic acidosis
- Fractures: CT and XR
- Vascular injuries: Doppler ultrasound to assess for pulses in crushed extremities followed by CT angiography
- Laboratory analysis: CBC, renal function, electrolytes, CK, lactate, PT/INR, PTT, fibrinogen
- Hyperkalemia, hypocalcemia, acute kidney injury, increase in CK/lactate common
Treatment
- Prehospital
- Administer intravenous fluids before releasing the crushed extremity8
- Obtaining a baseline ECG and treat electrolyte abnormalities
- Amputation is an absolute last resort if the patient is unable to be extricated17,18
- Tourniquet placement prior to release of entrapped extremity remains controversial.17,19
- Joint Trauma System (JTS) recommends application only if it has been >2 hours since entrapment, and if fluid resuscitation is not immediately available20
- Renal Disaster Relief Task Force and International Search and Rescue Advisory Group advise that application of tourniquets should only be used in cases of hemorrhage as utilization increases the risk of adverse events (i.e. neurologic damage and thrombosis)20,21
- Resuscitation
- Lactated ringers > Normal saline due to reduced need for urinary alkalinization22
- Place foley and target urine output >300 mL/hr
- Electrolyte abnormalities
- Hyperkalemia: Obtain an ECG
- Stabilization: Calcium gluconate 2 g over 5-10 min.
- Potassium shifting: Insulin 10u with 25-50 g of Dextrose 50 (D50)
- Hypocalcemia should not be immediately corrected as calcium supplementation may lead to deposition in necrotic muscle tissue and calcium may continue to be released from muscles and will normalize over time9,23
- Hyperkalemia: Obtain an ECG
- Electrolyte abnormalities
- Hyperkalemia: Obtain an ECG
- Stabilization: Calcium gluconate 2 g over 5-10 min.
- Potassium shifting: Insulin 10u with 25-50 g of Dextrose 50 (D50)
- Hypocalcemia should not be immediately corrected as calcium supplementation may lead to deposition in necrotic muscle tissue and calcium may continue to be released from muscles and will normalize over time9,23
- Hyperkalemia: Obtain an ECG
- Renal Failure
- Fluid resuscitation
- Urinary alkalinization to goal of pH >6.5
- Sodium bicarbonate to treat serum acidosis not routinely recommended but may be considered in cases where normal saline is only fluid available24
- Renal replacement therapy indicated for acidosis, electrolyte abnormalities, anuria16
- Prophylactic dialysis is not recommended as myoglobin is too large of a protein for many standard dialysis machines.25
Disposition
- Need for dialysis, severe electrolyte abnormalities or acute renal failure => ICU
- Hemodynamic instability or polytrauma => ICU
- Uncomplicated fractures and rhabdomyolysis => Step down status for frequent neurovascular checks
- Mild rhabdomyolysis requiring IVF => General medicine
- Patients without signs of significant kidney injury or rhabdomyolysis who can reliably take PO and have mild symptoms without underlying injuries can likely be discharged home after fluid resuscitation in emergency department and down-trending CK
Pearls
- Morbidity from crush injuries is a product of force and time
- Patients most commonly present with myalgias
- Conduct a primary and secondary survey, and treat associated injuries as appropriate
- Lactated Ringers is preferred to normal saline in resuscitation
- Treat hyperkalemia, permit hypocalcemia
- Prehospital care can have a huge impact

A 42-year-old man presents to the emergency department after a motor vehicle collision. He has no medical problems. He sustained a crush injury to his left leg and a prolonged extraction time. He is agitated and reporting significant pain. His left leg is mottled with significant ecchymoses and gross deformity below the left knee. Pulses are intact. Which of the following is a complication of this injury?
A) Acute tubular necrosis
B) Membranoproliferative glomerulonephritis
C) Renal papillary necrosis
D) Renal vein thrombosis
Answer: A
This individual is presenting with a traumatic crush injury of his lower extremity with intact pulses. Even in the absence of vascular compromise, these injuries result in significant tissue breakdown and necrosis, with massive cellular lysis and systemic release of intracellular components. The breakdown of muscle tissue can lead to rhabdomyolysis. This is typically characterized by a significant elevation in serum creatine kinase. Other laboratory findings include myoglobinuria and downstream effects of massive cell lysis, including hypocalcemia, hyperkalemia, hyperphosphatemia, and elevated uric acid. The breakdown of heme-containing myoglobin and subsequent deposition of circulating heme protein is nephrotoxic and can cause heme pigment acute tubular necrosis. Acute kidney injury in rhabdomyolysis is a common complication. Other complications include acid-base derangements and disseminated intravascular coagulation in severe cases. The prevention and management of acute kidney injury from rhabdomyolysis require aggressive fluid resuscitation with isotonic saline titrated to urine output to promote increased renal perfusion, dilute heme pigment concentration, and increase potassium excretion.

Membranoproliferative glomerulonephritis (B) is a pattern of glomerular injury caused by immune complex deposition, typically as a result of autoimmune disease or chronic infection such as hepatitis C. Renal papillary necrosis (C) is commonly found in patients with analgesic nephropathy. Renal vein thrombosis (D) is a form of venous thromboembolism that can occur in patients with nephrotic syndrome or newborns with inherited thrombophilia.
FOAMed Resources
- http://www.emdocs.net/emdocs-cases-evidence-based-recommendations-for-rhabdomyolysis/
- https://www.acep.org/imports/clinical-and-practice-management/resources/ems-and-disaster-preparedness/disaster-preparedness-grant-projects/cdc—blast-injury/cdc-blast-injury-fact-sheets/crush-injury-and-crush-syndrome/
References
- Peiris D. A historical perspective on crush syndrome: the clinical application of its pathogenesis, established by the study of wartime crush injuries. J Clin Pathol. 2017;70(4):277-281.
- Bywaters EG, Beall D. Crush Injuries with Impairment of Renal Function. Br Med J. 1941;1(4185):427-432.
- Oda J, Tanaka H, Yoshioka T, et al. Analysis of 372 patients with Crush syndrome caused by the Hanshin-Awaji earthquake. J Trauma. 1997;42(3):470-475; discussion 475-476.
- Tanaka H, Oda J, Iwai A, et al. Morbidity and mortality of hospitalized patients after the 1995 Hanshin-Awaji earthquake. Am J Emerg Med. 1999;17(2):186-191.
- Bartels SA, VanRooyen MJ. Medical complications associated with earthquakes. Lancet. 2012;379(9817):748-757.
- Kica J, Rosenman KD. Multi-source surveillance for work-related crushing injuries. Am J Ind Med. 2018;61(2):148-156.
- Veenstra J, Smit WM, Krediet RT, Arisz L. Relationship between elevated creatine phosphokinase and the clinical spectrum of rhabdomyolysis. Nephrol Dial Transplant. 1994;9(6):637-641.
- https://www.acep.org/imports/clinical-and-practice-management/resources/ems-and-disaster-preparedness/disaster-preparedness-grant-projects/cdc—blast-injury/cdc-blast-injury-fact-sheets/crush-injury-and-crush-syndrome/. Published June 2009. Accessed February 3, 2023. ACoEpAHP.
- Chavez LO, Leon M, Einav S, Varon J. Beyond muscle destruction: a systematic review of rhabdomyolysis for clinical practice. Critical Care. 2016;20(1):135.
- Genthon A, Wilcox SR. Crush syndrome: a case report and review of the literature. J Emerg Med. 2014;46(2):313-319.
- Goodman AD, Got CJ, Weiss AC. Crush Injuries of the Hand. J Hand Surg Am. 2017;42(6):456-463.
- Stahl K, Rastelli E, Schoser B. A systematic review on the definition of rhabdomyolysis. J Neurol. 2020;267(4):877-882.
- Cervellin G, Comelli I, Benatti M, Sanchis-Gomar F, Bassi A, Lippi G. Non-traumatic rhabdomyolysis: Background, laboratory features, and acute clinical management. Clin Biochem. 2017;50(12):656-662.
- Chen CY, Lin YR, Zhao LL, et al. Clinical spectrum of rhabdomyolysis presented to pediatric emergency department. BMC Pediatr. 2013;13:134.
- Eken C, Yigit O. Traumatic asphyxia: a rare syndrome in trauma patients. Int J Emerg Med. 2009;2(4):255-256.
- Wald R, Quinn RR, Luo J, et al. Chronic dialysis and death among survivors of acute kidney injury requiring dialysis. JAMA. 2009;302(11):1179-1185.
- Sever MS, Vanholder R. Management of crush victims in mass disasters: highlights from recently published recommendations. Clin J Am Soc Nephrol. 2013;8(2):328-335.
- Macintyre A, Kramer EB, Petinaux B, Glass T, Tate CM. Extreme measures: field amputation on the living and dismemberment of the deceased to extricate individuals entrapped in collapsed structures. Disaster Med Public Health Prep. 2012;6(4):428-435.
- Sever MS, Vanholder R, Disasters RoIWGoRftMoCViM. Recommendation for the management of crush victims in mass disasters. Nephrol Dial Transplant. 2012;27 Suppl 1:i1-67.
- https://jts.amedd.army.mil/assets/docs/cpgs/Crush_Syndrome_PFC_28_Dec_2016_ID58.pdf. Accessed 21 February 2023. CS-PFCJTSCPGPDAa.
- https://www.insarag.org/wp-content/uploads/2018/12/ATTACHMENT_C_The_Medical_Management_of_the_Entrapped_Patient_with_Crush_Syndrome_10_2019_-_Final.pdf. Accessed 15 August 2023. ISaRAGTmmotepwcsPOAa.
- Cho YS, Lim H, Kim SH. Comparison of lactated Ringer’s solution and 0.9% saline in the treatment of rhabdomyolysis induced by doxylamine intoxication. Emerg Med J. 2007;24(4):276-280.
- Chatzizisis YS, Misirli G, Hatzitolios AI, Giannoglou GD. The syndrome of rhabdomyolysis: complications and treatment. Eur J Intern Med. 2008;19(8):568-574.
- Somagutta MR, Pagad S, Sridharan S, et al. Role of Bicarbonates and Mannitol in Rhabdomyolysis: A Comprehensive Review. Cureus. 2020;12(8):e9742.
- Petejova N, Martinek A. Acute kidney injury due to rhabdomyolysis and renal replacement therapy: a critical review. Critical Care. 2014;18(3):224.







