Author: Christopher J. Nelson, MD (EM Resident Physician, UTSW, Dallas, TX) // Reviewed by: Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 28-year-old male presents as a transfer from an urgent care with report of left-hand injury. He is a construction worker and was using a table saw when he injured his left hand. The amputated part is wrapped in a plastic bag. He is right-handed.
Triage vital signs include BP 123/74, HR 98, T 98.8F oral, RR 16, SpO2 97% on RA.
Imaging from outside hospital are below:

What is the patient’s diagnosis? What’s the next step in your evaluation and treatment?
Answer: Finger Amputation
Background:
- An average of over 46,400 finger amputations occurred in the US from 1997 to 20162
- Bimodal distribution – below the age of 5 year and over the age of 65 years2
- Doors and power saws are the most common mechanisms2
- Goals of treatment are to restore function, sensation, durability, and proper nail growth
- Improper treatment may lead to loss of function, pain, and poor cosmetic outcome3
Anatomy:
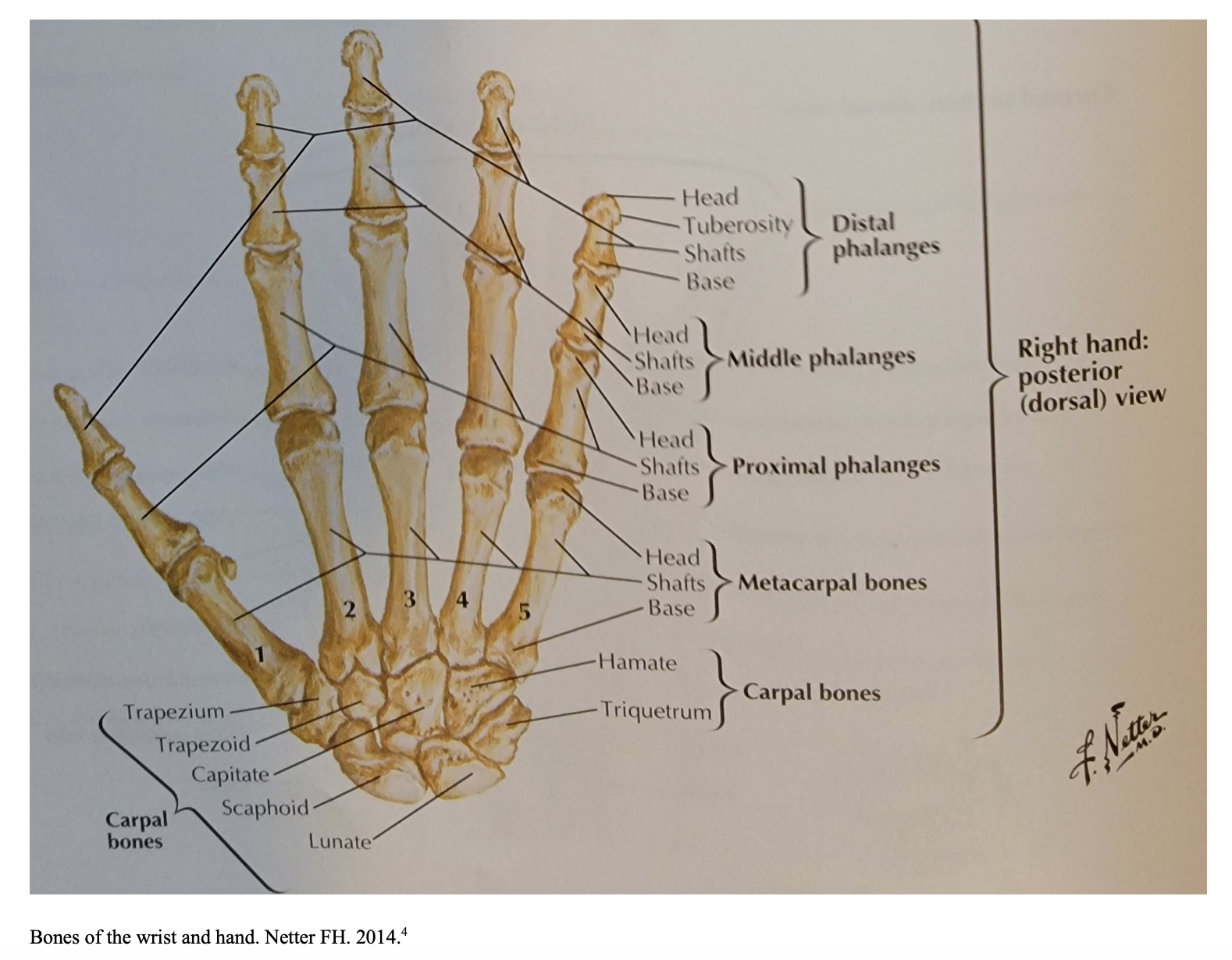
- The hand consists of phalanges, metacarpal bones, and carpal bones
- Each finger has a distal, middle, and proximal phalanges
- The thumb has distal and proximal phalanges
- Finger joints (distal to proximal):
- Distal interphalangeal joints (DIP)
- Proximal interphalangeal joints (PIP)
- Metacarpophalangeal joints (MCP)
- Thumb joints
- Interphalangeal joint
- Metacarpophalangeal joint
- Carpometacarpal joint
- Neurovascular components run on the lateral aspects of the digits
- Naming digits is less likely confused than numbering – Thumb, index, long, ring and pinky
- Varying numbering systems can otherwise lead to miscommunication
History and Exam:
- Mechanism of injury
- Time of injury
- Other signs of injury (amputation may be a distracting injury to other injuries)
- Amputated digit cold vs. warm (important for reimplantation time)5
- Tetanus status
- Dominant hand
- History of blood thinners
- History of diabetes and smoking, which are predictors of poor wound healing7
- Examination of each digit’s sensation and strength
- Isolating and examining extension/flexion of MCP, PIP, and DIP to assess flexor and extensor tendon involvement
- Careful examination of nailbed/subungual hematoma
- Treatment of nailbed injuries important to avoid cosmetic and functional loss in fingertip injuries6
Differential:
- Finger amputation, fingertip amputation, finger laceration, nail/nailbed laceration, ring avulsion injury, crush injury
ED Evaluation:
- Hand and finger x-rays, including amputated part
- Consider preop labs
- CBC, BMP, PT/INR, PTT
- Time of amputations to guide reimplantation viability
- Time between amputation/loss of blood supply to the digit prior to surgery
- 12 hours of warm ischemia5
- Time without cooling of amputated digit
- 24 hours of cold ischemia5
- Cooling of the digit
- Covered in saline-moistened gauze in a sealed bag on ice
- Cooling of the digit
- 12 hours of warm ischemia5
- Time between amputation/loss of blood supply to the digit prior to surgery
Management:7
- Stabilize patient and perform primary and secondary survey
- Irrigate amputated part and injury site with saline and wrap in moist sterile gauze
- Palpate for obvious foreign body
- Place amputated part in bag; place this in water with crushed ice
- Direct contact with ice can cause irreversible damage to cells7
- Limit handling of amputation when possible
- Administer cefazolin 2 grams or clindamycin for penicillin allergy7,8
- No difference in infection rates (antibiotics vs. none) if injury is a fingertip amputation with planned surgical management9
- Tetanus prophylaxis
- Analgesics – Local vs. systemic
- Local
- Digital blocks
- Lidocaine 1% vs. Bupivacaine 0.5%
- Digital blocks
- Systemic
- May consider when multiple injuries or insufficient analgesic effect with digital blocks
- Fentanyl, hydromorphone, or morphine
- Local
- Early hand surgery consultation
- General indications for replantation10
- Thumb
- Multiple digits
- Single digit distal to the insertion of the flexor digitorum superficialis tendon
- Pediatric amputations
- General contraindications for reimplantation10
- Severe crush/avulsion injuries
- Single digit proximal to the insertion of the flexor digitorum superficialis tendon
- Prolonged ischemic time
- Reimplantation counseling
- 80% viability after reimplantation10
- ~50% motion compared to normal10
- Requires prolonged physical therapy (PT)
Disposition:
- Admit for patients with infection or if patient will undergo reimplantation
- Discharge those with controlled bleeding and distal phalanx amputation
Pearls:
- History involves mechanism, cold/warm ischemic time, tetanus, hand dominance, medical issues
- Imaging should include amputated part
- Place amputated part in moist gauze, avoid direct ice contact
- Consider both systemic and local analgesics
- Early surgical consult
- Council patient on realistic outcomes, 80% viability, 50% motion and prolonged PT
References:
- Hacking, C. Traumatic finger amputation. Case study, Radiopaedia.org. Accessed on 24 December 2021) DOI: 0.53347/rID-37376.
- Reid DBC, Shah KN, Altorai AEM, et al. Epidemiology of Finger Amputations in the United States From 1997 to 2016. Jornal of Hand Surgery Global Online. 2019;1(2):45-51. DOI:10.1016/j.jhsg.2019.02.001.
- Kawaiah A, Thakur M, Garg S, et al. Fingertip Injuries and Amputations: A Review of the Literature. Cureus. 2020;12(5):e8291. doi:10.7759/cureus.8291.
- Netter FH. Atlas of Human Anatomy. Philadelphia, PA: Saunders/Elsevier, 2014;6:443.
- Chim H, Maricevich MA, Carlsen BT, et al. Challenges in replantation of complex amputations. Semin Plast Surg. 2013;27(4):182-189. doi:10.1055/s-0033-1360585.
- Tos P, Titolo P, Chirila NL, et al. Surgical treatment of acute fingernail injuries. J Orthop Traumatol 2012;13:57.
- Lloyd MS. et al. Preoperative management of the amputated limb. Emerg Med J. 2005;22(7):478-80.
- Rodriguez L, Jung HS, Goulet JA, et al. Evidence-based protocol for prophylactic antibiotics in open fractures: improved antibiotic stewardship with no increase in infection rates. J Trauma Acute Care Surg. 2014;77(3):400-407. doi: 10.1097/TA.0000000000000398. PMID: 25159242.
- Rubin G et al. The use of prophylactic antibiotics in treatment of fingertip amputation: A randomized prospective trial. Am J Emerg Med 2015 May; 33:645.
- Rebowe RE, Tannan SC. Digit Replantation. [Updated 2021 Sep 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. https://www.ncbi.nlm.nih.gov/books/NBK448187/ Accessed on 01/10/2022.







