Author: Jo-Anna Palma, MD (EM Resident Physician, UTSW, Dallas, TX) // Edited by: Brit Long, MD (@long_brit, EM Attending Physician, San Antonio, TX), Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 69-year-old female presents to your emergency department complaining of shortness of breath, orthopnea, and lower extremity swelling. Her symptoms started 5 days ago and have progressively worsened. She denies history of heart failure or use of diuretics. The patient tells you she had a pacemaker placed 3 years ago for a complete heart block. She hands you her pacemaker identification card indicating that she has a single chamber pacemaker.
Triage vital signs (VS): BP 100/72, HR 73, RR 25, SpO2 88% on RA that improve to 93% with 3L NC.
Triage EKG: ventricular pacing spikes followed by QRS complexes.

The patient appears uncomfortable. She has jugular venous distension, crackles at the lung bases, and 2+ lower extremity pitting edema. A 4 cm well healed scar is noted on her left upper chest and you are able to feel the pacemaker underneath her skin. The site is clean, dry, intact.
What is the diagnosis? What is your next step in evaluation? What are some the types of pacemaker complications you should be evaluating for?
Diagnosis: Pacemaker Syndrome
Pacemaker Basics: There are two types of cardiac implantable electronic devices: Pacemaker and Automatic Implantable Cardioverter Defibrillator (AICD). Both are made up of two elements: a pulse generator and lead(s). The pulse generator contains a battery pack and control unit. One or two leads are connected to the pulse generator and function as a bridge to the heart muscle [1]. These wires will detect the electrical activity of the heart, send the information to the control unit, and deliver electrical impulses to stimulate depolarization.
- Single chamber pacemakers contain one lead:
- The lead can terminate in the right atrium or in the right ventricle.
- Right atrial leads are placed for patients with sinus node disease.
- Right ventricular leads are placed for patients with atrial fibrillation.
- Dual chamber pacemakers contain two leads:
- One lead terminates in the right atrium and the second in the right ventricle.
- Used to help control the timing between the atrial and the ventricular contraction or depolarization [1, 2].
- Biventricular chamber pacemakers contain three leads.
- Think of a biventricular chamber as a dual chamber system with an additional lead.
- The additional lead courses through the coronary sinus into the left ventricle.
- Biventricular chambers are typically used in patients with advanced heart failure.
- AICD: An AICD works in a similar way but has the additional capability of functioning as a defibrillator and delivering high pulse electrical shocks when it detects life-threatening heart rhythms. These include ventricular tachycardia or ventricular fibrillation [3]. A shock is delivered that will convert these rhythms to sinus rhythms.
Background and Anatomy:
- Pacemaker Syndrome (PMS): Pacemaker syndrome is defined as the cardiovascular and neurological consequence of either atrial-ventricular (AV) or ventricular-ventricular (VV) dyssynchrony after pacemaker implantation and is purely iatrogenic [1].
- Pacemaker syndrome is thought to occur at an incidence of 18.3%, and data show no predilection to gender [4].
- In order to meet diagnostic criteria, a patient with a ventricular paced rhythm must meet one of the following criteria [5]:
- (a) develop congestive symptoms in the setting of retrograde ventricular-atrial (VA) conduction.
- (b) systolic blood pressure reduction of greater than or equal to 20 mmHg during pacing that is associated with symptoms.
- Single-chamber devices where both pacing and sensing occur at the level of the ventricle carry higher risk of development [6].
- In other words, when the atria are not responsible for telling the ventricle when to contract, the latter will follow the preset impulse from the generator.
- Native physiology allows for forward flow of blood when the atria contracts, the tricuspid valve opens, and the right ventricle relaxes and fills.
- Mistiming of these contractions can be deleterious, as the atrial chamber may contract when the atrioventricular valves are closed.
- Often misdiagnosed, this syndrome can also occur in the setting of dual chamber pacing, as has been demonstrated when the conduction to the atria is impeded or delayed leading to a primarily ventricular paced system. Examples of such cases include lead displacement, lead fracture, or initiation of anti-arrhythmic drugs that may alter the threshold for capture [1,7].
- Regardless of the inciting factor, adequate flow through the heart is compromised and the chambers are forced to pump against higher filling pressures.
- This results in both decreased cardiac output and venous congestion mirroring symptoms of heart failure with reduced ejection fraction.
Clinical Presentation:
- History and Physical:
- Neurological symptoms include dizziness, syncope, confusion, and weakness [5,7].
- Cardiovascular symptoms are reflected as dyspnea, orthopnea, lower extremity edema, orthostatic hypotension, and jugular venous distension [5,7].
- Vital signs:
- Low blood pressure
- Increased respiratory rate
- Hypoxia
- Canon-a waves: this is a non-specific finding but occurs when the atria contracts against a closed tricuspid valve [2].
- Physical exam:
- Jugular venous distension
- Right upper quadrant pain
- Abdominal distension
- Liver pulsation
- Diagnostic tests:
- EKG: often shows pacing spikes followed by capture, but dyssynchrony between the p wave and QRS complex. Think of this as a “pacemaker induced” third-degree heart block [1]. It is not uncommon to identify retrograde p waves in individuals with pacemaker syndrome. These findings are consistent with atrioventricular dissociation, as the atrium depolarization is occurring after ventricular depolarization.

-
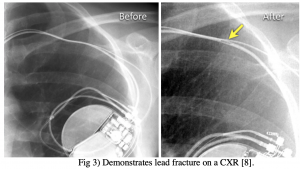
- CXR: When considering the diagnosis of pacemaker syndrome, it is important to follow the pacemaker leads carefully to ensure integrity and proper placement.
- Treatment: Pacemaker syndrome requires re-programming of the pacemaker, adjustment of pacemaker parameters, or addition of leads as heart failure treatments such as diuretics are ineffective [1].
Differentials:
- Pacemaker Malfunction: In order to properly function, a pacemaker must successfully accomplish two tasks: pace and sense. Successful pacing results in depolarization of the cardiac chamber. Successful sensing results in the recognition of the native cardiac activity (whether it be appropriate or inappropriate). If the intrinsic cardiac activity is sensed, it should not prompt the pulse generator to deliver an impulse. Therefore, pacemaker malfunctions can be broken down into two categories.
-
- Pacing malfunction
-
-
- Failure to pace: the pacemaker fails to deliver a stimulus resulting in return of underlying rhythm. The EKG will show pacer spikes with appropriate P waves or QRS complexes and intermittently return to the irregular rhythms for which the pacemaker was initially placed.
-

-
-
- Failure to capture: the pacemaker delivers a stimulus, but the stimulus does not result in cardiac depolarization. The EKG will show pacer spikes that are not followed by P waves or QRS complexes. This may be caused by post-operative lead displacement, wire insulation breaks, or wire fractures.
-

-
- Sensing malfunction
-
-
- Failure to sense: The native cardiac activity is appropriate, but the electrical impulse is delivered erroneously. The EKG will show intermittent and inconsistent pacer spikes (i.e. within a QRS complex). This may be caused by wire insulation breaks, electrolyte abnormalities, or anti-arrhythmic medications.
-

-
-
- Oversensing: Inappropriate sensing of non-cardiac external signals (such as skeletal muscle contraction). The pacemaker will identify this external signal as “appropriate” and will thus, not send out an impulse when one is required. The sensitivity of a pacemaker can be decreased to avoid oversensing.
-

- Twiddler Syndrome: Twiddler syndrome occurs when the pulse generator is rotated within the subcutaneous pocket resulting in lead(s) fracture, dislodgement, displacement, or coiling. The ultimate consequence of such manipulation causes pacemaker malfunction. Manipulation of the pulse generator can be accidental and/or intentional. Clinical presentation varies and is largely dependent on the location of the leads after manipulation. Two common locations of displacement are discussed below [4,11]:
- Ipsilateral phrenic nerve: this will result in contraction of the diaphragm with intermittent hiccups and unintentional respirations.
- Brachial plexus: this will result in unintentional arm twitching. Treatment requires lead uncoiling, repositioning, or replacement.

- Others: Pneumothorax, Cardiac Perforation, Battery depletion, Lead fracture
General Diagnostic Basics:
- EKG findings in a functional pacemaker will demonstrate the following:
- Pacemaker spike before the p wave indicates atrial pacing.
- Pacemaker spike before the QRS indicates ventricular pacing.
- Pacemaker before the p wave, before the QRS, or before both indicates dual chamber pacing.
- Chest X-Ray (CXR):
- A CXR is a quick and reliable tool for identification and assessment in any patient with cardiac symptoms and help identify the type and manufacturer of implantable cardiac devices when patients are unable to provide this information.
- The CaRDIA-X algorithm was developed to aid in the radiological identification of these devices that follow 6 different steps:
- Gather information from the patient – if information is available call the manufacturer: Medtronic, St. Jude Medical, Boston Scientific, Biotronik, Sorin
- If device manufacturer is not identified – obtain a CXR
- Identify the radiopaque alphanumeric codes (ANC)
- If un-identifiable–look at the CXR characteristics to help differentiate between AICD and pacemaker
- More than 1 radiopaque shadow + high voltage coil = AICD
- Look at the shape and orientation of the battery, identify the leads and their integrity and count the number of leads.
- Analyze the shape of the pacemaker/ICD casing, sometimes referred to as the can. The shape of the can is unique amongst different manufacturers and will thus assist in further identification/differentiation.
- Reference for complete CaRDIA-X: http://www.ianchristoph.com/physician-resources-2/device_id.pdf
- Pacemaker Interrogation: A magnet can be placed over the pulse generator site and allows for the pacemaker to convert to a fixed-rate mode, where it functions independent of the patients’ intrinsic cardiac activity. This will allow for evaluation of rate and appropriateness of capture. It is important to distinguish between a pacemaker and an AICD, as magnets placed over an AICD will de-active the system.
- Obtain lab tests including electrolytes and cardiac markers: troponin, brain natriuretic peptide (BNP).
Management
- As with any patient that is hemodynamically unstable, Airway/Breathing/Circulation are a priority.
- If the patient has an unstable rhythm, revert back to Advanced Cardio Life Support (ACLS).
- External pacing pads and defibrillators may still be used in patients with permanent pacemakers and AICDs, however, the pads should be placed in the anterior-posterior position 2.5-8.0 cm away from the implanted device [12].
Disposition
- If there is concern for pacemaker/AICD malfunction or associated cardiovascular concern, cardiology consultation is warranted.
- Admission is recommended if any of the following criteria are present [13]:
- Hemodynamic instability
- Lead system interruption is identified
- Signs of infection at the pocket site of AICD/pacemaker
- Reversible causes (i.e. electrolyte abnormalities) of cardiac abnormalities are identified
Pearls
- Pacemaker syndrome is the clinical consequence of cardiac chamber mistiming.
- It is defined by its cardiovascular and neurological symptoms as they relate to pacemaker function.
- It is most commonly seen in individuals with ventricular paced systems.
- Any patient who is suspected to have pacemaker syndrome will likely be refractory to heart failure treatment and will require acute pacemaker intervention to treat the underlying problem.


A 70-year-old man with a recently placed pacemaker presents with palpitations. An electrocardiogram obtained shows the above pattern. You suspect the issue is related to the pacemaker device. What is the most likely etiology of the patient’s symptoms?
A) Failure to capture
B) Failure to defibrillate
C) Failure to pace
D) Failure to sense
Answer: D
The ECG above suggests failure to sense or undersensing of the pacemaker. Failure to sense occurs when the pacemaker cannot detect the heart’s intrinsic electrical activity. It is a common presentation of pacemaker malfunction and can occur when a lead is loose, dislodged, or broken. Undersensing can also occur if the lead is placed in a poor conduction zone of the heart. Complete failure to sense sometimes occurs when the sensing threshold is programmed too high. Patients often present with palpitations or symptoms similar to a previously diagnosed dysrhythmia. This can manifest with certain findings on ECG, including unnecessary pacing spikes that follow too closely behind the QRS complexes.

Failure to capture (A) occurs when a pacemaker’s pulse generator fires appropriately, but at a current that is not strong enough to initiate cardiac depolarization. On ECG, pacing spikes will be present at the appropriate locations, but not followed by a QRS complex. Failure to defibrillate (B) would be incorrect. ICD devices have the ability to both defibrillate and act as a pacemaker, but pacemakers alone do not have the ability to defibrillate. Failure to pace (C) or oversensing occurs when electrical signals from the body or other indwelling devices interfere with the pacemaker, causing it to incorrectly inhibit the pulse generator.
Further Reading:
#FOAMed
- emDocs – Pacemaker and ACID management in the Emergency Department: http://www.emdocs.net/pacemaker-and-aicd-management-in-the-emergency-department/
- EM:RAP – Troubleshooting Pacemakers & ICD’s: https://www.emrap.org/episode/emraplive9/grandrounds
- LITFL – Pacemaker malfunction: https://litfl.com/pacemaker-malfunction-ecg-library/
- REBEL EM – Pacemaker Basics: https://rebelem.com/pacemaker-basics/
References
- Link MS, Hellkamp AS, Estes NA, et al. “High Incidence of Pacemaker Syndrome in Patients with Sinus Node Dysfunction Treated with Ventricular-Based Pacing in the Mode Selection Trial (MOST).” Journal of the American College of Cardiology, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/15172414/.
- Dalong Chen and Pei-Ying Pai. Cannon A Wave. Retrieved September 10, 2020, from https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.108.833095
- Jerrard, G., Berberian, J., & Zeserson, E. (2019, February 05). Pacemaker Basics for the Emergency Physician. Retrieved September 10, 2020, from https://www.emra.org/emresident/article/pacemaker-basics/
- Bouthillet, T. (2016, April 29). The Basics of Paced Rhythms. Retrieved September 11, 2020, from https://www.ecgmedicaltraining.com/the-basics-of-paced-rhythms-part-1/
- Keroes, J., Lieberman, D., & Erickson, B. (2020). Introduction to Pacemaker Rhythms. Retrieved September 10, 2020, from https://ekg.academy/pacemaker-rhythms
- Farmer, D Michael, et al. “New Concepts in Pacemaker Syndrome.” Indian Pacing and Electrophysiology Journal, Indian Pacing and Electrophysiology Group, 1 Oct. 2004, ncbi.nlm.nih.gov/pmc/articles/PMC1502063/
- Aboyme, Andrew, et al. “ECG Interpretation for Suspected Pacemaker Syndrome.” Journal of the American College of Cardiology, 24 Mar. 2020, onlinejacc.org/content/75/11_Supplement_1/3234.
- Elsinger, F., Smithuis, R., & Spijkerboer, A. (2018). Cardiovascular devices. Retrieved September 10, 2020, from https://radiologyassistant.nl/cardiovascular/devices/cardiovascular-devices
- Chin, A., Taher, A., Thomas, A., Bigham, B., Thoma, B., & Woods, R. (2016, May 28). Pacemaker Essentials: How to Interpret a Pacemaker ECG. Retrieved September 10, 2020, from https://canadiem.org/pacemaker-essentials-interpret-pacemaker-ecg/
- Salahuddin, Mohammad, et al. “The Pacemaker-Twiddler’s Syndrome: an Infrequent Cause of Pacemaker Failure.” BMC Research Notes, BioMed Central, 20 Jan. 2016, ncbi.nlm.nih.gov/pmc/articles/PMC4721019/
- Clements, P A D. “Hazards of Performing Chest Compressions in Collapsed Patients with Internal Cardioverter Defibrillators.” Emergency Medicine Journal, British Association for Accident and Emergency Medicine, 1 July 2003, emj.bmj.com/content/20/4/379.
- Tintinalli, Judith. Tintinalli’s Emergency Medicine. McGraw-Hill Education, 2015.
- Ganz, L., Piccini, J., & Downey, B. (2020). Cardiac implantable electronic devices: Long-term complications. Retrieved September 10, 2020, from https://www.uptodate.com/contents/cardiac-implantable-electronic-devices-long-term-complications
- Iqbal, Arshad Muhammad. “Pacemaker Syndrome.” StatPearls [Internet]., U.S. National Library of Medicine, 27 Apr. 2020, ncbi.nlm.nih.gov/books/NBK536976/.
- Jacob S, Shahzad MA, Maheshwari R, et al. “Cardiac Rhythm Device Identification Algorithm Using X-Rays: CaRDIA-X.” Heart Rhythm, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/21220049/.
- Knight, B., Levy, S., & Downey, B. (2020). Implantable-Cardioverter Defibrillators. Retrieved September 10, 2020, from https://www.uptodate.com/contents/implantable-cardioverter-defibrillators-beyond-the-basics
- Olshansky, B., Ganz, L., & Downey, B. (2018). Pacemakers (Beyond the Basics). Retrieved September 10, 2020, from https://www.uptodate.com/contents/pacemakers-beyond-the-basics
- Wiper, Andrew. “Pacemaker Syndrome – a Forgotten Diagnosis?” The British Journal of Cardiology, 1 Jan. 2008, bjcardio.co.uk/2008/01/pacemaker-syndrome-a-forgotten-diagnosis/.







