Author: Amber Cibrario, DO (EM Attending Physician, San Antonio, TX), Zachary Baker, DO (EM Attending Physician, San Antonio, TX), Rachel Bridwell, MD (@rebridwell, EM Resident Physician, SAUSHEC / San Antonio, TX) // Reviewed by: Alex Koyfman, MD (@EMHighAK) and Brit Long, MD (@long_brit)
Welcome to EM@3AM, an emDOCs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 3-month-old male brought is in by his parents for increased work of breathing for the last 4 days. The patient has had no fevers, rash, vomiting, diarrhea, rhinorrhea, or sick contacts. He was born full term without complications, is fully vaccinated, and has no familial medical history. He is breast fed and typically feeds every 3 hours. The patient has had a decrease in PO intake over the last 3 days with prolonged feeding times.
Triage vital signs (VS): BP 85/50, HR 152, RR 56, SpO2 92% on room air, oral temp 99.9. The patients is tachypneic with weak cry, but has normal pink color. There is a 4/6 holosystolic murmur, with 2+ femoral and brachial pulses. He has suprasternal and intercostal retractions with wheezes. There is also palpable hepatomegaly.
What’s the next step in your evaluation and treatment?
Answer: Heart failure from septal defect1-16
Epidemiology:1,2
- 12,000-35,000 cases of heart failure (HF) in patients less than 19 years old are diagnosed in the US each year.
- 11,000-14,000 HF related hospitalizations in children per year in the US
- Congenital Heart Disease (CHD) affect nearly 1% of―or about 40,000―births per year in the United States.
- The prevalence of CHDs is increasing.
- Ventricular septal defect (VSD) most common defect
- 25% of babies with a CHD have a critical CHD.
- Critical CHD requires surgery or other procedures in their first year of life.
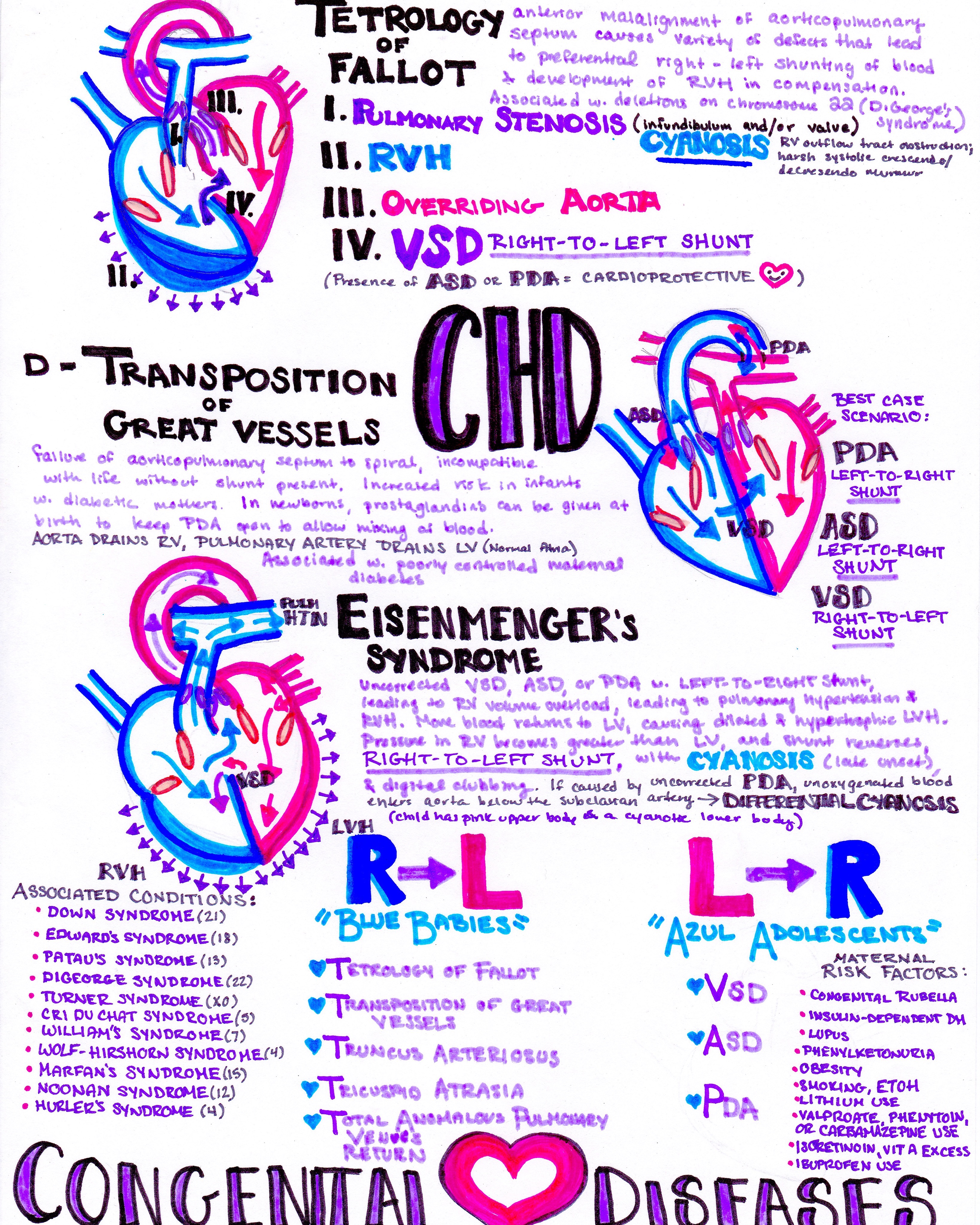
Physiology:3-6
- Prior to birth, pulmonary vascular resistance is high
- Majority of blood from the right ventricle passes right-to-left across the ductus arteriosus
- 8-10% of the fetal cardiac output perfusing the lungs.
- At birth, the lungs expand and systemic oxygenation rises when respirations begin
- Pulmonary vasodilatation decreases pulmonary vascular resistance
- Systemic vascular resistance increases with ligation of the umbilical
- Following the closure of the ductus arteriosus and foramen ovale, the systemic arterial (left side) and pulmonary (right side) systems are isolated series in parallel.
- A ventricular septal defect, atrial septal defect (ASD), or patent ductus arteriosus (PDA) permits left to right shunting.
- If large left to right shunts are untreated, pulmonary hypertension and Eisenmenger’s syndrome (reversal of shunt) may occur.
Clinical Presentation:7,8
- Clinical presentations of left-to-right shunts vary from patients from asymptomatic to florid heart failure.
- Variation depends on the size of the shunt and its resulting physiologic effects.
- Typical clinical findings include age > 1 month to 6 months, tachypnea, tachycardia, diaphoresis, poor weight gain, and hepatomegaly.
- Get a feeding history: < 3 ounces of formula per feed or > 40 minutes per breast correlates with moderate-severe HF.
- Typical Murmurs:
- VSD
- Harsh, holosystolic
- ASD
- Fixed splitting of S2
- PDA
- Continuous machinery-like murmur inferior to left clavicle
- Capillary refill is delayed only in critically ill patients with shunt.
- VSD
Evaluation:
- Utilize pediatric assessment triangle: Appearance, work of Breathing, Color.
- On history assess for fussiness, difficulty breathing, and poor feeding.
- Independently obtain RR and HR is sick infants; do not rely on triage vitals.
- Respiratory rate > 60 breaths per minute or irregular breathing is a sensitive sign for acute HF in infants.8
- Physical Examination Pearls.
- Cardiac: Assess for pulses in each extremity, capillary refill.
- Respiratory: cardiac presentations may present with wheezing
- Abdomen: Extent of Hepatomegaly can be a sign of HF
- Liver should be less than 2 cm from the right costal margin7
- Laboratory evaluation:7
- Blood glucose
- CBC—assess for anemia
- CMP—evaluate for electrolyte changes secondary to fluid overload as well as elevated liver associated enzymes secondary to congestive hepatopathy
- AST elevations may also evaluate for myocarditis
- Troponin– screening for myocarditis, but is not 100% sensitive
- BNP: ongoing debate about usefulness of this test, particularly in the ED setting:9,10,11
- BNP < 100pg/mL to identify significant congenital heart disease had a sensitivity of 100% and specificity of 98%.
- BNP > 132.5pg/mL to detect hemodynamically significant left-to-right shunts has a 93% sensitivity and 100% specificity.
- BNP > 40pg/mL to differentiate cardiac from pulmonary causes of respiratory distress has an accuracy of 84%.
- Shunt fraction through PDA is the main determinant of plasma levels of natriuretic peptides in premature infants.
- In patients with ASDs or VSDs, BNP levels were mildly increased when compared with healthy age-matched controls. Shunt severity and pulmonary artery pressure are reflected by natriuretic peptide levels.
- Imaging
- CXR
- Concerns of cardiomegaly, pulmonary edema, infiltrate.
- Patients with left-to-right shunting also are at risk for viral pulmonary infections, especially respiratory syncytial virus.
- POCUS
- Evaluation for shunt using color flow may be possible but likely is outside purview of EM.
- Number of chambers, contractility, as well as potential presence of a pericardial effusion, B lines, or as pleural effusions are helpful with diagnosis.
- ECG
- Pink babies may also be secondary to arrythmias, myocarditis, or additional structural defects like anomalous Left Coronary Artery from the Pulmonary Artery (ALCAPA).
- CXR
Treatment:
- Medications:12-14
- Diuretics are the primary therapy. Oxygen supplementation +/- positive pressure, and vasopressors should also be considered in the ED.
- Mild HF requires diuretic initiation.
- 1 mg/kg of furosemide13
- Moderate-Severe HF requires diuretics, inotropes, and oxygen.
- Slower correction needed in these patients to match rate insidious rate of derangement rather than rapid deterioration that may be seen in other etiologies (i.e. myocarditis).
- ACE inhibitor, ARB, beta blockers, and mineralocorticoids receptor blockers may be subsequently added once patient returns to compensated state.
- Mild HF requires diuretic initiation.
- Vasopressors:7,12-15
- Milrinone – Reduce afterload & increases contractility
- Some experts say to start at 0.01mcg/kg/min but will likely need to titrate quickly for effect to 0.5mcg/kg/min.
- Not usually available in the ED.
- Dopamine – Also considered a first line for decompensated HF in pediatrics, but may increase SVR which would increase left to right shunt.
- Dose: 3-10 mcg/kg/min
- Dobutamine – Readily available in ED in crash carts
- Dose: 5-1 mcg/kg/min IV continuous infusion initially and titrate
- Titrate 5-10 mcg/kg/min for inotropic effects
- Epinephrine – Increases SVR at high doses. If true inotropes unavailable, lower dose will provide predominant beta agonism over alpha.7,12
- Dose:01–0.5 mcg/kg/min start low and titrate
- Escalating doses lead to have greater alpha agonism, increasing SVR and left to right shunt.
- Avoid phenylephrine or norepinephrine – increase SVR due to predominant alpha agonism.
- Oxygen/PPV7,16
- PPV promotes alveolar recruitment, improves lung compliance, and leads to decreased LV preload and afterload.
- Oxygen is a potent pulmonary vasodilator, increasing pulmonary blood and worsening pulmonary edema so titrate oxygen carefully
- Goal oxygen saturation is >85%.
- Milrinone – Reduce afterload & increases contractility
- Diuretics are the primary therapy. Oxygen supplementation +/- positive pressure, and vasopressors should also be considered in the ED.
Disposition:
- Pediatric ICU
Pearls:
- Always consider HF in a wheezing child, especially at 1-6 months of age.
- < 3 ounces of formula per feed or > 40 minutes per breast is affiliated with moderate-severe HF.
- Do not trust triage vital signs, obtain your own respiratory rate.
- Examine for hepatomegaly.
- Initiate diuretics.
- Be more tolerant of lower oxygen saturations.

From Dr. Katy Hanson at Hanson’s Anatomy:

A 5-week-old infant suffers from dyspnea and fluid overload, but not cyanosis. Auscultation reveals a loud, holosystolic murmur at the lower left sternal border. You suspect a congenital cardiac defect. Echocardiography would most likely show which of the following abnormalities?
A) Aorta is connected to the right ventricle
B) Pulmonary artery is connected to the left ventricle
C) Ventricular septal defect in the membranous portion
D) Ventricular septal defect in the muscular portion
Answer: C
The most common congenital heart defect is a ventricular septal defect (VSD), one of the acyanotic congenital heart diseases. Defects occur in the ventricular septum, the “wall” between the right and left ventricle. This septum is comprised of an inferior muscular part and a superior membranous part. The majority of VSDs occur in the membranous part, near the atrioventricular node. A pansystolic murmur is nearly pathognomonic for VSD. Occurrence and severity of clinical manifestations depend on the size of the defect. Spontaneous closure occurs in the first six-months of life in up to 40% of affected infants. If present, symptoms may be mild or severe, but usually present as congestive heart failure due to a significant left-to-right intracardiac shunt with resultant pulmonary hypertension. Pharmacotherapy is recommended in these patients. However, surgical correction is typically necessary if the patient fails medical management or shows evidence of pulmonary hypertension (elevated pulmonary artery pressure).
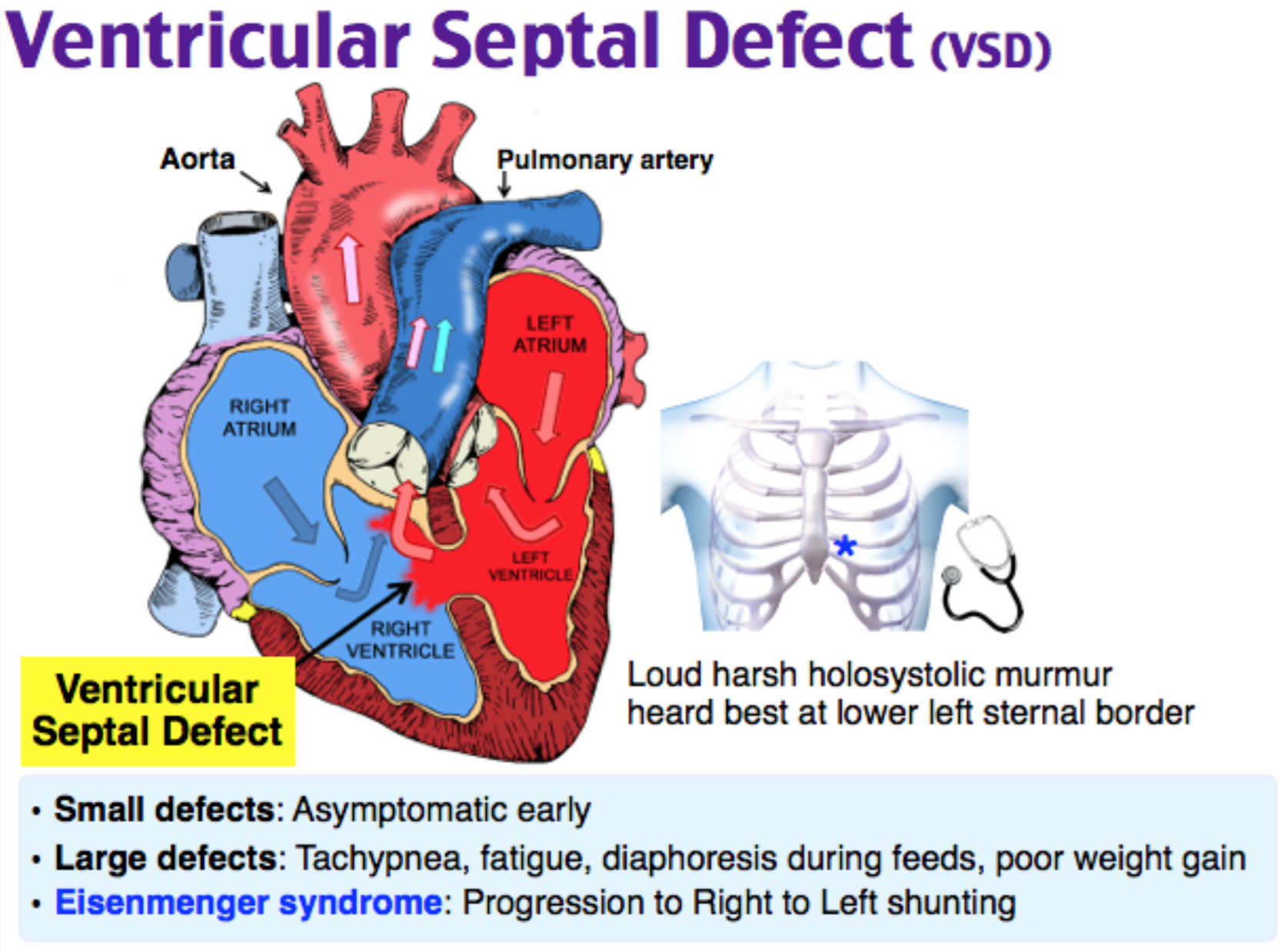
Transposition of the great arteries (A and B) is usually a cyanotic, not acyanotic, congenital cardiac defect in which the aorta is connected to the right ventricle and the pulmonary artery is connected to the left ventricle. It is a rare defect, affecting only 5% of all infants with congenital defects. If a VSD is concurrent, a loud pansystolic murmur is likely present, however, the infant would still have significant cyanosis. The presenting signs and symptoms suggest VSD, however, the majority of them occur in the membranous, not muscular (D), portion of the ventricular septum.
Further Reading:
FOAM Resources
Emergency Medicine Cases: Congenital Heart Disease
PEM PLAYBOOK: Undifferentiated Sick Neonate
References
- Pearson GD; Hsu DT. Heart Failure in Children: Part I: History, Etiology, and Pathophysiology. Heart Failure, U.S. National Library of Medicine, 2009, pubmed.ncbi.nlm.nih.gov/19808316/.
- Data and Statistics on Congenital Heart Defects. https://www.cdc.gov/ncbddd/heartdefects/data.html. Accessed September 15, 2020
- Rossano JW; Kim JJ; Decker JA; Price JF; Zafar F; Graves DE; Morales DL; Heinle JS; Bozkurt B; Towbin JA; Denfield SW; Dreyer WJ; Jefferies JL. Prevalence, Morbidity, and Mortality of Heart Failure-Related Hospitalizations in Children in the United States: A Population-Based Study. Journal of Cardiac Failure, U.S. National Library of Medicine, 2012, pubmed.ncbi.nlm.nih.gov/22633303/.
- Iwamoto HS, Teitel D, Rudolph AM. Effects of birth-related events on blood flow distribution. Pediatr Res. 1987 Dec;22(6):634-40. doi: 10.1203/00006450-198712000-00004. PMID: 3431945.
- Teitel DF, Iwamoto HS, Rudolph AM. Changes in the pulmonary circulation during birth-related events. Pediatr Res. 1990 Apr;27(4 Pt 1):372-8. doi: 10.1203/00006450-199004000-00010. PMID: 2342829.
- Jain A, Mohamed A, Kavanagh B, Shah PS, Kuipers BCW, El-Khuffash A, Mertens L, Jankov RP, McNamara PJ. Cardiopulmonary Adaptation During First Day of Life in Human Neonates. J Pediatr. 2018 Sep;200:50-57.e2. doi: 10.1016/j.jpeds.2018.04.051. Epub 2018 May 24. PMID: 29803302.
- Strobel AM, Lu LN. The Critically Ill Infant with Congenital Heart Disease. Emerg Med Clin North Am. 2015;33(3):501-518. doi:10.1016/j.emc.2015.04.002
- Ross RD, Bollinger RO, Pinsky WW. Grading the severity of congestive heart failure in infants. Pediatr Cardiol. 1992 Apr;13(2):72-5. doi: 10.1007/BF00798207. PMID: 1614922.
- Davlouros PA, Karatza AA, Xanthopoulou I, Dimitriou G, Georgiopoulou A, Mantagos S, Alexopoulos D. Diagnostic role of plasma BNP levels in neonates with signs of congenital heart disease. Int J Cardiol. 2011 Feb 17;147(1):42-6. doi: 10.1016/j.ijcard.2009.07.029. Epub 2009 Aug 26. PMID: 19712988.
- Holmström H, Hall C, Thaulow E. Plasma levels of natriuretic peptides and hemodynamic assessment of patent ductus arteriosus in preterm infants. Acta Paediatr. 2001 Feb;90(2):184-91. doi: 10.1080/080352501300049406. PMID: 11236049.
- Eindhoven, J., Van den Bosch, A., Boersma, E., & Roos-Hesselink, J. (2013). The usefulness of brain natriuretic peptide in simple congenital heart disease – a systematic review. Cardiology in the Young, 23(3), 315-324. doi:10.1017/S1047951112001205
- Wessel DL. Managing low cardiac output syndrome after congenital heart surgery. Crit Care Med. 2001 Oct;29(10 Suppl):S220-30. doi: 10.1097/00003246-200110001-00004. PMID: 11593065.
- Engle MA, Lewy JE, Lewy PR, Metcoff J. The use of furosemide in the treatment of edema in infants and children. Pediatrics. 1978 Nov;62(5):811-8. PMID: 724325.
- Costello JM, Almodovar MC. Emergency Care for Infants and Children with Acute Cardiac Disease. Clin Pediatr Emerg Med. 2007;8(3):145-155. doi:10.1016/j.cpem.2007.06.005
- Kantor PF, Mertens LL. Clinical practice: heart failure in children. Part II: current maintenance therapy and new therapeutic approaches. Eur J Pediatr 2010; 169:403.
- Tkacova R, Rankin F, Fitzgerald FS, Floras JS, Bradley TD. Effects of continuous positive airway pressure on obstructive sleep apnea and left ventricular afterload in patients with heart failure. Circulation. 1998 Nov 24;98(21):2269-75. doi: 10.1161/01.cir.98.21.2269. PMID: 9826313.







