Author: Brett Bartels, MD (EM Resident Physician, UTSW) // Reviewed by: Brit Long, MD (@long_brit) and Alex Koyfman, MD (@EMHighAK)
Welcome to EM@3AM, an emDocs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 30-year-old male with no medical history presents to the ED after a motor vehicle accident. He complains of chest pain and shortness of breath. He is alert, speaking in 1-2 word responses, and appears in moderate respiratory distress.
Exam reveals BP 102/68, HR 136, RR 26, Temp 98.2, SpO2 91% on room air. He has normal left sided breath sounds, but none on the right. Heart exam is normal, and his abdomen is soft. FAST is negative, but no lung sliding is seen with ultrasound examination of the right thorax. His trachea is deviated left, and increased JVD is noted.
What is this patient’s presentation consistent with? What is your next step in management?
Answer: Pneumothorax (specifically a tension pneumothorax)
Anatomy
- The pleural space is a potential space between the visceral pleura, attached to the lungs, and the parietal pleura lining the chest wall.
- Typically only filled with very small amounts of serous fluid, the pleural space can trap air with no means of outlet.
- Accumulation of air leads to compression of the lung parenchyma and affects the mechanics of ventilation.
- Pneumothoraces can be classified by size based on the distance between the lung margin and the chest wall on imaging: very small (<1cm), small (<3cm), and large (>3cm).
Background
- Air can enter the pleural space through the holes in the lung parenchyma, bronchial tree, or externally through the chest wall in a traumatic injury.
- A pneumothorax can be symptomatic, but the true danger lies in a tension pneumothorax, when a one-way valve effect allows air into the pleural space but it cannot escape.
- Increased pressure and volume can quickly overwhelm the lung’s ability to inflate, exert pressure on the heart and vasculature, and cause hemodynamic instability or death.
Causes
- Primary spontaneous – No underlying lung disease
- Classically tall, thin males
- Marfan syndrome
- Ehlers Danlos
- Homocystinuria
- Alpha-1 antitrypsin deficiency
- Secondary spontaneous – History of underlying lung disease
- Blebs
- COPD
- Asthma
- Pneumocystis jirovecii pneumonia
- Lung abscess
- Pulmonary infarction
- Malignancy
- Radiation necrosis
- Interstitial lung disease
- Cystic fibrosis
- Catamenial pneumothorax (endometriosis of pleura)
- Traumatic – May be open (injury through the chest wall into the pleural space) or closed (chest wall remains intact). Occult pneumothoraces are common in trauma, when not clinically suspected or found on initial imaging.
- Penetrating thoracic trauma
- Blunt trauma – 10% of blunt chest trauma patients in one prospective trial found to have pneumothorax, of which 68% were occult.2
- Tracheo-bronchial tree rupture
- Esophageal rupture
- Pulmonary laceration
- Commonly associated injuries include rib fractures, hemothorax, pulmonary contusion, and pneumomediastinum.
- Iatrogenic
- Central line placement
- Nasogastric tube placement
- Percutaneous biopsy
- Acupuncture
- Endoscopic perforation of esophagus
- Barotrauma (Mechanical ventilation, Scuba divers, etc.)
History
- Chest pain, often pleuritic and may be radiating to the ipsilateral shoulder.
- Likely to complain of shortness of breath, which may be sudden-onset or gradual.
- Cough, anxiety, fatigue, and upper abdominal pain are less common complaints.
- Of 100 patients with spontaneous pneumothorax in a study from Thailand, common symptoms included dyspnea (73%), chest pain (68%), pleuritic pain (46%), cough (20%), and fever (13%).3
- Tension pneumothorax is more likely to occur in a trauma patient.
- Ask about history of conditions such as COPD, asthma, Marfan, and HIV.
- Take a social history to assess for smoking, vaping, and drug use.
Exam
- Perform primary survey in trauma and ill-appearing patients. Avoid intubation if suspecting pneumothorax and the patient is protecting his/her airway and has no airway obstruction.
- Tension pneumothorax can present with tachycardia, hypotension, tachypnea, and hypoxia.
- Breath sounds may be diminished on one side. This may be more difficult to notice in small spontaneous pneumothoraces. Hyper-resonance to percussion and reduced chest expansion may also be observed.
- Tension pneumothorax may also have elevated JVD and tracheal deviation to the contralateral side.
- In traumatic etiologies of pneumothorax, always assess for other injuries. Do not anchor on only the pneumothorax.
Differential
- Pulmonary: Pneumothorax, PE, Pneumonia, Pleural Effusion, COPD, Asthma, Malignancy, Bronchitis, Lung abscess, Empyema, Right mainstem bronchus intubation
- Cardiovascular: Myocardial ischemia/ACS, Pericarditis, Myocarditis, Aortic dissection, CHF
- GI: GERD, Esophageal spasm, Mallory-Weiss tear, Boerhaave’s syndrome
- Other: Rib fracture, Flail chest, Shingles, Anxiety, Diaphragmatic injury, Costochondritis
- Artifacts on imaging: Skin folds, Clothing, Bullous Emphysema, Blebs
Diagnostics
- Tension pneumothorax is a clinical diagnosis and should be made prior to any imaging.
- Plain film – An upright PA chest x-ray is a standard first-line test, though can be a poor screening test in trauma. One prospective study of post-traumatic pneumothoraces demonstrated sensitivity of 20.9% and specificity 98.7%.4 Films in expiration do not improve diagnostic accuracy. Pneumothorax may be indicated by:
- Lack of lung markings extending to the pleura at the chest wall.
- May see complete deflation of lung.
- In a supine film, may see a deep, dark sulcus at the costophrenic angle, referred to as the “deep sulcus sign”.

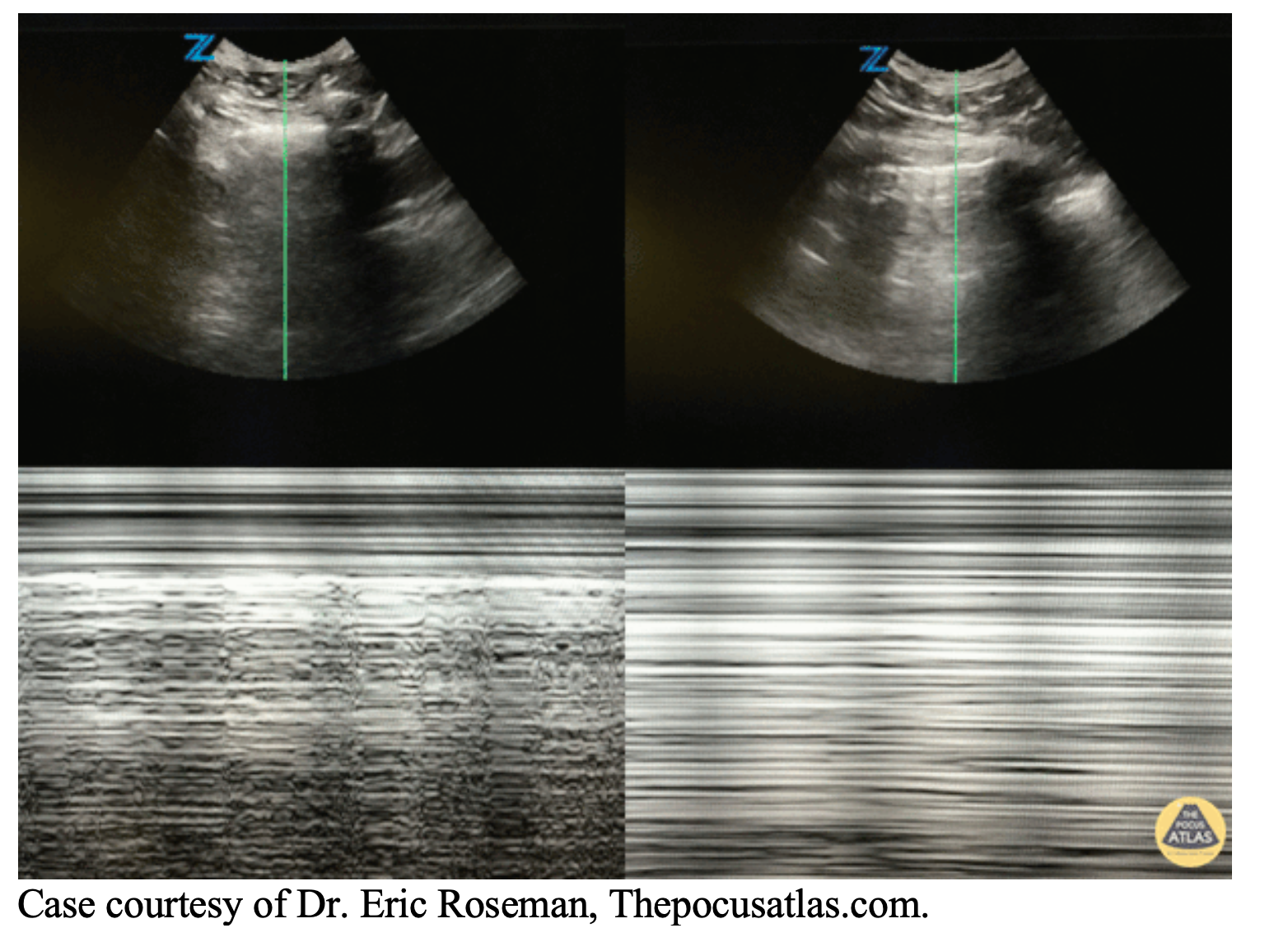
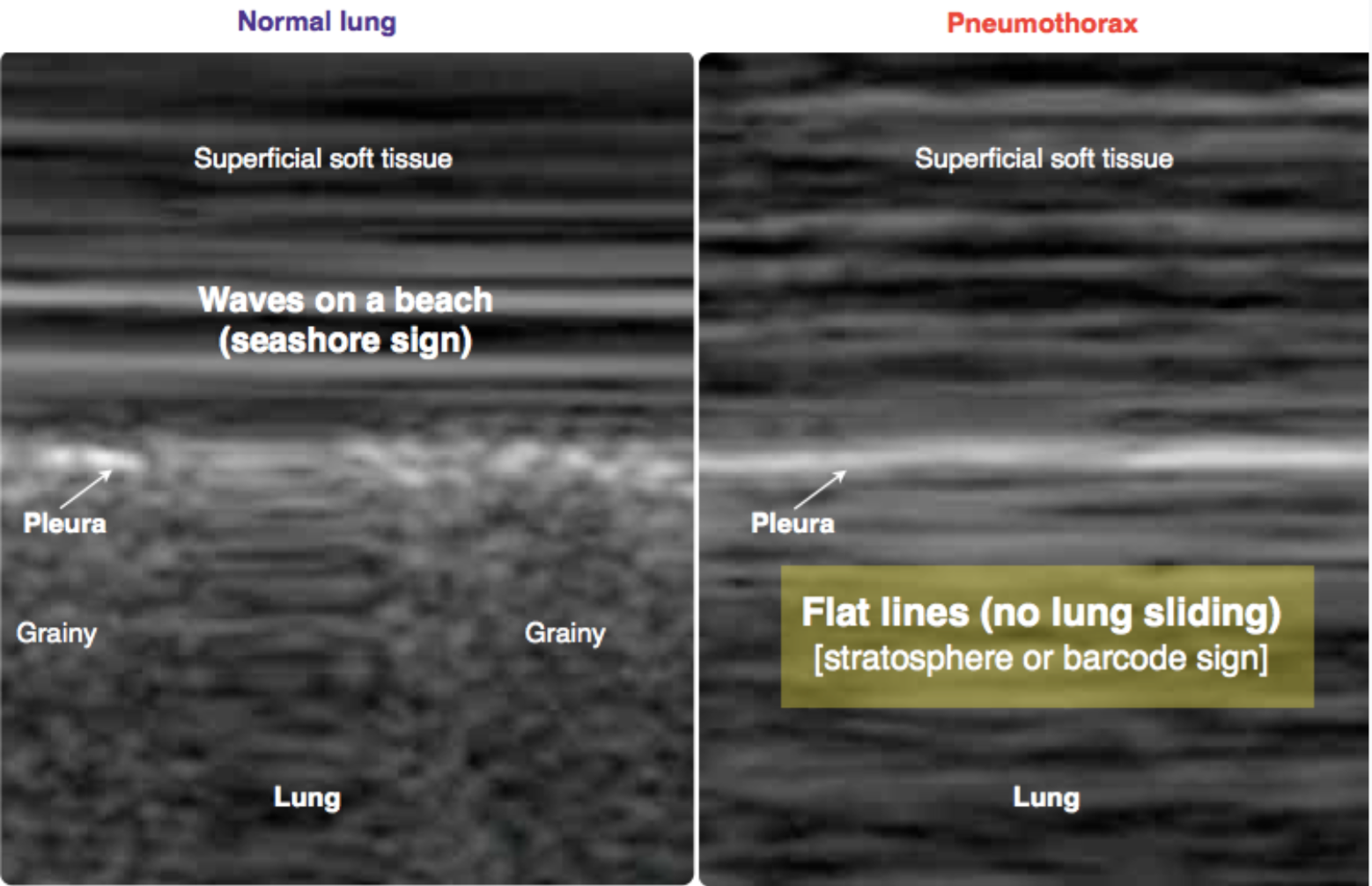
- Ultrasound – M-mode is used to assess for lung sliding between rib spaces. As air rises, this is best accomplished anteriorly when the patient is supine. Normal lung sliding is often described as a “seashore sign”. The absence of lung sliding, or a “bar code sign”, indicates a likely pneumothorax. See this US Probe post for lung point, this US Probe for occult pneumothorax identified by US, REBEL EM for more.
- Blunt trauma – Sensitivity 86-98%, Specificity 97-100%5
- ICU patients without trauma – Sensitivity 95.3%, Specificity 91.1%6
- In the image below, the seashore sign due to normal lung sliding is seen on the left, compared to a barcode sign indicating pneumothorax on the right.
- CT
- Gold standard for accurate evaluation, though may be unnecessary when considering acuity, pre-test probability, resources, and radiation.
- Particularly useful for assessing small pneumothoraces, in addition to underlying lung disease such as blebs.
Management
- Tension pneumothorax should be diagnosed clinically and treated immediately with needle decompression.
- Use a 14-gauge needle, at least 5 cm long, with a syringe to aspirate. Alternatively, perform finger thoracostomy for decompression.
- A pigtail catheter may be left in place, attached to suction or a Heimlich valve.
- Placement at the 4th/5th intercostal space in the anterior axillary line has lower failure rates compared to the traditional 2nd intercostal space in the mid-clavicular line.9
- Definitive management for a tension pneumothorax or large air leak may require a chest tube connected to suction.
- Give analgesics first if you have time.
- Anesthetize and prep the skin around the 5th intercostal space in the mid- or anterior axillary line.
- Make your incision at the rib, then advance with your finger and Kelly clamps over the superior aspect of the rib, through the pleura into the pleural space.
- Insert the tube through the tract, angled cephalad.
- Connect to the drainage device with water seal, hooked to suction.
- Secure the tube with sutures, cover with an occlusive bandage, and confirm correct placement with a chest x-ray.
- Administration of 100% oxygen will increase rate of pleural air resorption by approximately 4-fold. The natural rate of reabsorption of intrapleural air is 1-2% of lung volume per day.11
- Patients with a small primary pneumothorax (<3cm between lung margin and chest wall) may be observed on supplemental oxygen for 4 hours, then repeat chest x-ray. If symptoms and pneumothorax have improved, they may return for 24-hour follow up, with weekly follow up imaging until resolution. A recent randomized control trial of 316 patients with moderate-to-large uncomplicated primary spontaneous pneumothorax showed lung re-expansion at 8 weeks in 98.5% of patients who underwent interventional management, compared to 94.4% who were randomized to a watch and wait conservative approach. This could suggest non-inferiority of conservative management for this subset of patients.12
- Secondary pneumothoraces are generally treated with a chest tube and admission. The exception is asymptomatic very small pneumothoraces (<1cm interpleural distance), which may be treated with oxygen and observation, with close follow up for repeat chest x-ray in 12-24 hours.
- Persistent air leak requires evaluation of the drainage system. If concern for bronchial injury, surgical evaluation is recommended.
- Recurrent pneumothorax may benefit from pleurodesis.
- Complications:
- Obstructive Shock
- Hypoxemic respiratory failure
- Iatrogenic pneumothorax
- Intercostal vessel hemorrhage
- Hemothorax
- Empyema
- Chest tube malfunction
- Re-expansion injury
- Re-expansion pulmonary edema
Disposition
- Patients with uncomplicated spontaneous pneumothorax showing improvement both symptomatically and on follow-up x-ray may be managed conservatively and discharged home with close follow up. Resolution may take up to 8 weeks.
- Admit any patient requiring a needle decompression or chest tube.
- Patients should avoid air travel and diving until fully resolved.
Take Home Points
- Pneumothorax is due to air accumulating in the pleural space.
- Maintain a high index of suspicion in trauma patients with hemodynamic instability, or in mechanically ventilated patients with acute changes in vitals and vent pressures.
- Tension pneumothorax is a clinical diagnosis. Diagnose quickly, and treat immediately with a needle and/or chest tube in the 5th intercostal space, anterior axillary line.
- POCUS is fast, cost-effective, and highly sensitive and specific for pneumothorax.
- Small primary pneumothoraces may be observed while on oxygen for 4 hours. before discharge home if improving. All others will require chest tube or pigtail catheter and admission.


A 20-year-old healthy man presents to the emergency department with shortness of breath after a stab wound to the chest. Ultrasound finding of his left chest using M-mode is shown above. Based on his ultrasound, which of the following is the most likely diagnosis?
A) Hemothorax
B) Pericardial effusion
C) Pneumothorax
D) Pulmonary edema
Answer: C
This patient’s clinical scenario and ultrasound findings are consistent with pneumothorax. Pneumothorax, or air in the pleural cavity, is a common finding after penetrating or blunt chest trauma that can lead to rapid decompensation of the patient if not identified and treated appropriately. An open chest wound can allow influx of air during the negative pressure phase of the inspiratory cycle, causing a progressively enlarging volume of air in the thorax. Patients may complain of chest pain or shortness of breath due to this diminished functional lung capacity. On exam, the provider may note diminished breath sounds or crepitus. Definitive diagnosis requires imaging; ultrasound has been shown to have sensitivity and specificity similar to that of computed tomography scans for pneumothorax and can outperform inspiratory chest radiographs in detecting occult pneumothorax. On ultrasound, the lung point sign (separation point of pleural layers at the margin of the pneumothorax where both lung sliding and absence of sliding are seen in one image), barcode sign (on M-mode), or absence of lung sliding may be seen to identify a pneumothorax. Treatment depends on the size of the pneumothorax and patient symptoms, with small asymptomatic pneumothoraces being treated with supplemental oxygen and larger or symptomatic pneumothoraces requiring tube thoracostomy for evacuation of the air and prevention of progression to a tension pneumothorax.
Hemothorax (A) may present in a similar clinical scenario, however, ultrasonography would reveal a homogenous anechoic effusion due to the collection of fluid. Additionally, a “spine sign,” or visualization of the thoracic spine, may be present due to the increased penetration of ultrasound waves through the fluid compared to air. Pericardial effusion (B) could also present from penetrating chest trauma, however, the patient would have normal lung sounds, diminished heart sounds, jugular venous distention and ultrasound of the heart would show an anechoic effusion. Pulmonary edema (D) is more commonly seen in fluid overload states such as congestive heart failure and would present as B-lines on ultrasound (greater than 4 vertical “light beams” per lung field).
Further Reading:
FOAMed:
https://rebelem.com/ultrasound-detection-pneumothorax/
https://rebelem.com/what-is-the-best-anatomic-location-for-needle-thoracostomy/
https://foamcast.org/2016/03/19/episode-36-pneumothorax/
http://www.emdocs.net/us-probe-radiographically-occult-pneumothorax-identified-by-ultrasound/
https://litfl.com/emergency-thoracocentesis/
https://www.wikem.org/wiki/Pneumothorax_(main)
https://radiopaedia.org/articles/pneumothorax
References
- Cydulka RK, Cline DM, Ma OJ, Fitch MT, Joing S, Wang VJ. Tintinalli’s Emergency Medicine Manual, 8th Edition. New York: McGraw-Hill Education, 2017.
- Langdorf MI, Medak AJ, Hendey GW, et al. Prevalence and Clinical Import of Thoracic Injury Identified by Chest Computed Tomography but Not Chest Radiography in Blunt Trauma: Multicenter Prospective Cohort Study. Ann Emerg Med. 2015 Dec;66(6):589-600.
- Saiphoklang N, Kanitsap A. Prevalence, clinical manifestations and mortality rate in patients with spontaneous pneumothorax in Thammasat University Hospital. J Med Assoc Thai. 2013; 96(10):1290-1297.
- Kirkpatrick AW, Sirois M, Laupland KB, Liu D, Rowan K, Ball CG, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: The extended focused assessment with sonography for trauma (EFAST) J Trauma. 2004;57:288–95.
- Wilkerson RG et al. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med. 2010. PMID: 20078434.
- Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Chest. 1995;108;1345-8.
- Stone MB. Ultrasound diagnosis of traumatic pneumothorax. J Emerg Trauma Shock. 2008;1(1):19–20. doi:10.4103/0974-2700.41788
- Alrajab S, Youssef AM, Akkus NI, Caldito G. Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis. Crit Care. 2013 Sep 23;17(5):R208.
- Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonographic diagnosis of pneumothorax. J Emerg Trauma Shock. 2012;5(1):76-81. Doi:10.4103/0974-2700.93116
- Laan DV et al. Chest wall thickness and decompression failure: A systematic review and meta-analysis comparing anatomic locations in needle thoracostomy. Injury. 2016; 47: 797-804.
- MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010 Aug; 65 Suppl 2:ii18-31.
- Brown SGA, Ball EL, Perrin K, et al. Conservative versus interventional treatment for spontaneous pneumothorax. The New England Journal of Medicine. 2020;382(5):405-415, doi:10.1056/NEJMoa1910775.
- Zehtabchi S, Rios CL. Management of emergency department patients with primary spontaneous pneumothorax: needle aspiration or tube thoracostomy? Ann Emerg Med. 2008 Jan; 51(1):91-100, 100.e1.
- Inaba K, Lustenberger T, Recinos G, Georgious C, Velmahoa GC, Brown C, Salim A, Demetriades D, Rhee P. Does size matter? A prospective analysis of 28-32 versus 36-40 French chest tube size in trauma. J Trauma Acute Care Surg. 2012 Feb;72(2):422-7.









3 thoughts on “EM@3AM: Pneumothorax”
Pingback: REBEL Core Cast 33.0 - Needle Decompression - REBEL EM - Emergency Medicine Blog
Pingback: REBEL Core Cast 34.0 - Chest Tubes - REBEL EM - Emergency Medicine Blog
This study shows traumatic pneumothorax less than 35mm has 91% success rate without chest tube; which is a difference from the recommendation of most secondary pneumothorax treatment with chest tube
https://pubmed.ncbi.nlm.nih.gov/30629009/
https://www.cedars-sinai.org/content/dam/cedars-sinai/education/documents/fellowships/trauma-journal/2019/may-8-2019observing-pneumothoraces-the-35-millimeter-rule-is-safe-for-both-blunt-and-penetrating-chest-trauma.pdf