Author: Brit Long, MD (@long_brit, EM Attending Physician, San Antonio, TX) // Edited by: Alex Koyfman, MD (@EMHighAK, EM Attending Physician, UTSW / Parkland Memorial Hospital)
Welcome to EM@3AM, an emDocs series designed to foster your working knowledge by providing an expedited review of clinical basics. We’ll keep it short, while you keep that EM brain sharp.
A 62-year-old female patient presents with dysuria and frequency. You quickly order a urine dipstick. She has normal VS and denies fever, vomiting, and vaginal discharge. What do you need to consider when interpreting the urine dipstick or urinalysis?
Background:
– Urinalysis and urine dipstick are commonly ordered in the ED for a variety of conditions. However, it should only be ordered to assist your decision-making in the ED. What components make up urinalysis and dipstick, and where can we go wrong?
Color – Urine is normally a shade of yellow and transparent, dependent on several conditions. Higher pH and more concentrated urine is typically darker. The presence of mucous, epithelial cells, sperm, urinary crystals, and lotion/powders can result in a change of urine opacity. Color may change in several circumstances:

Specific Gravity – This is the amount of solute dissolved in the urine. Water possesses a specific gravity of 1.000. This measurement closely correlates to urine osmolality and measures the kidney’s ability to concentrate urine. A normal value ranges from 1.002 to 1.035. Values can suggest other conditions in the right clinical setting.

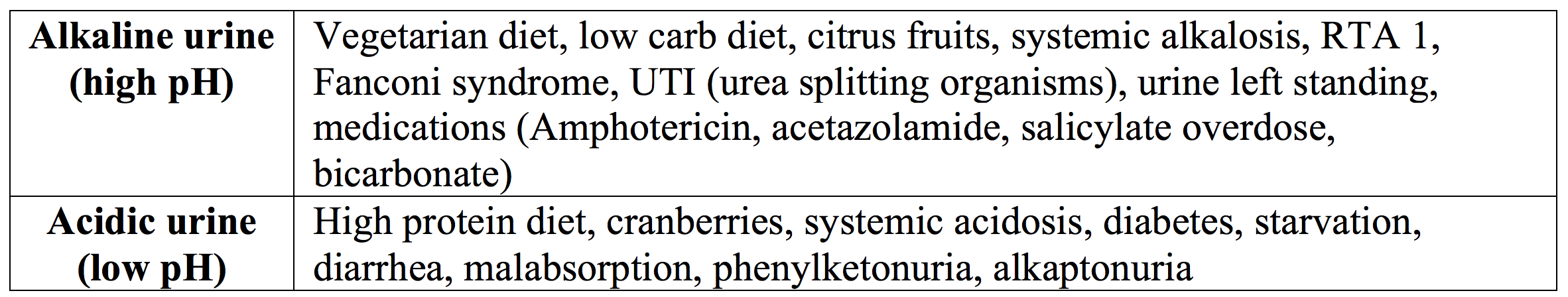
pH – Acid-base status is in part regulated through the kidneys. Normal urinary pH ranges from 5.5-6.5 (some say 4.5-8.0). The kidneys’ ability to regulate urinary pH plays an important role in several diseases, in particular urolithiasis and UTI.
Protein – The renal system normally excretes less than 150 mg of protein in 24 hours (10 mg/100 mL). The definition of proteinuria means urinary protein > 150 mg/day, with nephrotic syndrome > 3.5 g/day. Dipstick analysis uses a Bromophenol blue indicator dye, which is sensitive to albumin. However, it is less sensitive to Bence-Jones protein and globulins.
– True urinary protein elevation includes increased glomerular filtration, nephrotic syndrome, pyelonephritis, glomerulonephritis, hypertension, fever, cold exposure, stress, eclampsia, CHF, shock, orthostatic proteinuria, hypokalemia, Cushing’s syndrome, and drugs (NSAIDs, sulfonamides, penicillins, amphotericin).
– Bence-Jones protein is associated with multiple myeloma, lymphoma, and macroglobulinemia.
– False positive protein elevation may be due to concentrated urine, alkaline urine, bleach, acetazolamide, cephalosporins, and bicarbonate.
– False negatives can occur with acidic and dilute urine.
Leukocyte Esterase – This test correlates with the presence of whole or lysed white blood cells (WBCs) through detection of an enzyme present in WBCs. False positives occur with contaminated specimens, trichomonal infection, and medications/foods that color urine red. False negatives occur with recent antibiotic treatment, glycosuria, proteinuria, and high specific gravity.
Nitrites – This test correlates with the presence of bacteria that can convert urinary nitrates to nitrites (typically Gram-negative species such as E. coli and Klebsiella). Bacteria concentrations of 10,000 bacteria/mL urine are usually required to produce a positive test. This test can be falsely negative in drugs or food that color urine red, or with bacteria that do not convert nitrates to nitrites.
Hematuria – Dipstick and urinalysis can detect hemolyzed and non-hemolyzed blood in the urine. RBCs, free hemoglobin, and myoglobin contain pseudoperoxidase, which can catalyze chromogen oxidation, resulting in color change and positive urine testing for hematuria. Positive results can be due to hematuria from infection, trauma, urolithiasis, cancer, and bleeding disorders. Other causes include intravascular hemolysis, cold exposure, transfusion reactions, sickle cell crisis, and eclampsia. False negative results can occur with vitamin C, high urine specific gravity, and acidic urine.
Glucose – Not normally in the urine, as less than 0.1% of glucose filtered through the glomerulus appears in the urine. This equates to < 130 mg in 24 hours. Elevated serum glucose levels (diabetes) and reduced glucose reabsorption (renal tubular disease and pregnancy) can result in increased urinary glucose levels. Medications such as penicillins, cephalosporins, lithium, nitrofurantoin, steroids, thiazides, tetracycline, methyldopa, and phenothiazines may cause glycosuria. False negative tests can occur with vitamin C or fruit juices and false positives with hydrogen peroxide or bleach.
Ketones – Accumulate in serum as a result of incomplete fat metabolism. The final products are excreted in the urine. Urinary ketones are found in low carbohydrate diets, starvation states, diabetes (DKA), alcoholism, eclampsia, and hypothyroidism. It can also be found in overdose from isoniazid, insulin, and isopropyl alcohol. Most dipstick and urinalysis assessments use a nitroprusside test. This is sensitive to acetoacetic acid, but it is not as sensitive to beta-hydroxybutyric acid (the dominant ketone in DKA). False negatives can occur in DKA when beta-hydroxybutyric acid is the predominant ketone. False positive results occur in heavily pigmented urine and drugs like salicylates, phenothiazines, and captopril.
Bilirubin – Not normally present in urine of healthy patients. This can occur with liver disease before the onset of jaundice. Bilirubin is a product of RBC breakdown. Only the conjugated form can be excreted in the urine as bilirubin. High levels of conjugated bilirubin are present in liver disease (cirrhosis, hepatitis), pancreatic disease (carcinoma), biliary tract obstruction, and idiopathic jaundice of pregnancy. Hemolysis should not increase urinary bilirubin levels. False positives may be due to phenothiazines, and false negatives with vitamin C, rifampin, UV light exposure, and an old sample.
Urobilinogen – May be present at low levels (0.2-1 mg/dL). Diseases such as cirrhosis, hepatitis, hemolysis, and malaria can result in elevated levels. Levels are typically decreased in biliary obstruction, unlike with bilirubin above.
The following table gives you the false positives and false negatives all in one place for reference:

Further Reading:
- Long B, Koyfman A. The Lowly Urinalysis: How to Avoid Common Pitfalls. EP Monthly. Available at https://epmonthly.com/article/lowly-urinalysis-avoid-common-pitfalls/
- Simerville JA, Maxted WC, Pahira JJ. Urinalysis: A Comprehensive Review. Am Fam Physician.2005 Mar 15;71(6):1153-1162.
- Hanno PM, Wein AJ, Malkowicz SB. Clinical manual of urology. 3d ed. New York: McGraw-Hill, 2001.
- Sheets C, Lyman JL. Urinalysis.Emerg Med Clin North Am. 1986;4:263–80.
- Cadogan M. Urinalysis. LIFTL. https://lifeinthefastlane.com/investigations/urinalysis/.
- Kiel DP, Moskowitz MA. The urinalysis: a critical appraisal.Med Clin North Am. 1987;71:607–24.
- Benejam R, Narayana AS. Urinalysis: the physician’s responsibility.Am Fam Physician. 1985;31:103–11.







1 thought on “EM@3AM: Urinalysis/Urine Dipstick Components”
Pingback: Länkar v7- | Internmedicin