Today on the emDOCs cast, Jess Pelletier and Brit Long cover acute aortic occlusion.
Episode 104: Acute Aortic Occlusion
Background:
- AAO is a rare condition in which aortic blood flow is suddenly obstructed. May be due thrombosis or embolism; leads to potential ischemia of downstream tissue.
- Largest cohort study to date found that the mortality for AAO was 19.9% at 30 days.
- Associated with prolonged hospital stays and ⅔ of patients have complications of revascularization, including end-organ ischemia.
Epidemiology:
- Incidence7 to 5 cases per million people annually; typically impacts older adults between ages 60-70 years with cardiovascular comorbidities.
- Thrombosis of the native aorta due to atherosclerosis is the most common underlying etiology; may also involve thrombotic occlusion of a stent, graft, or stent-graft; secondary to an abdominal aortic aneurysm; via a dissection flap; or as a result of blunt abdominal trauma.
- Embolic cases of AAO are commonly associated with atrial fibrillation; may also be due to clot formation from ventricular aneurysm, due to low ejection fraction, or valvular disease, or tumor embolism.
Pathophysiology:
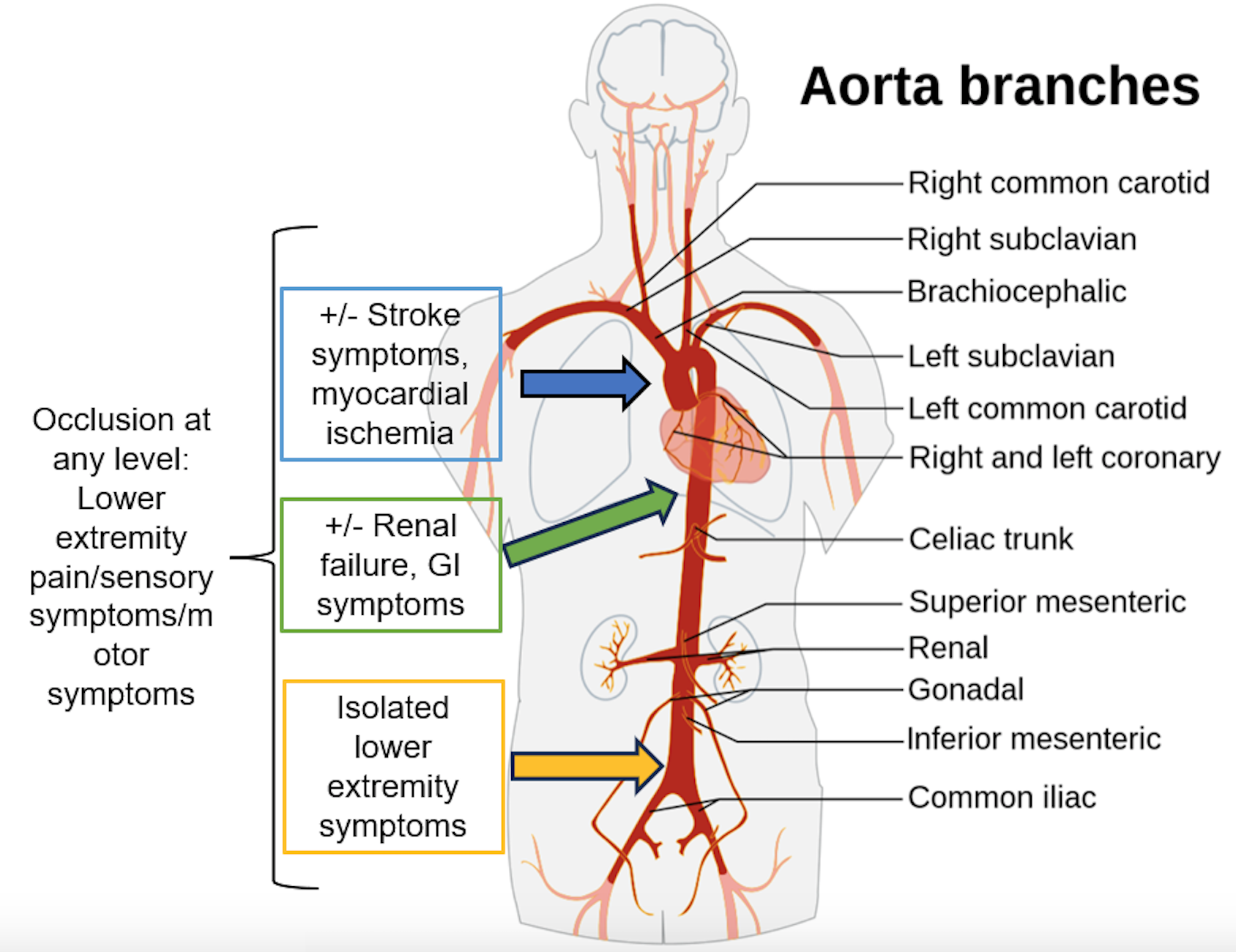
- AAO most commonly occurs below the renal arteries, leading to bilateral lower extremity symptoms, though occlusion of the aorta can occur at any level.
- Embolic occlusion occurs more rapidly than thrombotic occlusion and present with more severe symptoms.
Presentation:
- Presenting symptoms of AAO relate to the organs and structures with ischemia secondary to lack of perfusion.
- Acute lower limb ischemia is the most common presentation: pain, pallor, and poikilothermia.
- Lower limb weakness is the most common reason AAO patients seek care; may be misdiagnosed as a neurologic diagnosis before a vascular issue is recognized.
- Other symptoms: back pain, GI symptoms, oliguria or anuria , myocardial infarction, or stroke.
Diagnosis:
- Exam:
- Neurovascular: Strength, sensation, reflexes; lower extremity pulses, color (mottling, pallor, erythema, cyanosis), blisters, temperature, swelling, capillary refill.
- Cardiovascular: Evaluate for murmurs and irregularly irregular rhythm; signs of heart failure (gallop rhythm, JVP, rales, and peripheral edema).
- Abdomen: Presence of a pulsatile mass, tenderness.
- Testing:
- Imaging:
- CT angiogram of the chest, abdomen, pelvis. Highly sensitive. Determines site of occlusion, affected organs, complications.
- MRI can be diagnostic but typically not feasible.
- Point-of-care ultrasound (POCUS) should be performed in the unstable patient: occlusive thrombus in the aorta with absence of distal color flow in color and pulsed-wave Doppler modes
- ECG for arrhythmia
- CBC (leukocytosis, thrombocytopenia), coagulation panel, electrolytes, renal and liver function (AKI, liver injury), lactate (66% of patients; associated with increased mortality).
- Imaging:
- Key components: vascular surgery consultation, anticoagulation, pain control (ideally with opioids, but consider ketamine), maintaining normoxia, fluid resuscitation if necessary, and avoiding extremes of heart rate or blood pressure.
- Volume: Target euvolemia; may require IV fluids.
- Administer blood products if patient anemic/thrombocytopenic and critically ill.
- Anticoagulation: Unfractionated heparin is the agent of choice due to its short half-life and reversibility; should be administered in all patients even in the setting of preexisting antithrombotic or antiplatelet medication use.
- Vascular surgery specialist may recommend adding a prostacyclin analog (i.e., iloprost) since this may reduce morbidity and perioperative mortality.
- Intervention:
- Endovascular therapy with thrombo-embolectomy is commonly first-line; least invasive approach and most likely to be successful in relieving the occlusion.
- There are a wide range of options: thrombolysis, endovascular procedures, and open procedures (e.g., aortobifemoral bypass, axillofemoral bypass, or combinations of various methods).
- Disposition: OR or endovascular suite, followed by ICU.
Summary:
- AAO is associated with high morbidity and mortality and may be due to thrombosis or embolism.
- Most commonly affects older adults with cardiovascular comorbidities.
- Typical presentation is signs and symptoms of acute limb ischemia. Neurovascular assessment is essential. Patients may also present with GI tract or renal involvement.
- Misdiagnosis leads to delays in management and increases mortality
- Imaging modality of choice is CTA of the chest, abdomen, and pelvis, but POCUS may be helpful in unstable patients.
- Management includes consulting vascular surgery specialist, administering anticoagulation, pain control, fluid resuscitate if necessary, maintain normal oxygen saturation.
References:
- Grip O, Wanhainen A, Björck M. Temporal Trends and Management of Acute Aortic Occlusion: A 21 Year Experience. Eur J Vasc Endovasc Surg. 2019;58(5):690-696. doi:10.1016/j.ejvs.2019.05.018
- Na DH, Hwang D, Park S, Kim HK, Huh S. Treatment Outcomes and Risk Factors for In-Hospital Mortality in Patients with Acute Aortic Occlusion. Vasc Spec Int. 2018;34(2):19-25. doi:10.5758/vsi.2018.34.2.19
- Babu SC, Shah PM, Nitahara J. Acute aortic occlusion – Factors that influence outcome. J Vasc Surg. 1995;21(4):567-575. doi:10.1016/S0741-5214(95)70188-5
- Mohapatra A, Salem KM, Jaman E, et al. Risk factors for perioperative mortality after revascularization for acute aortic occlusion. J Vasc Surg. 2018;68(6):1789-1795. doi:10.1016/j.jvs.2018.04.037
- Isselbacher EM, Preventza O, Hamilton Black J, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease. J Thorac Cardiovasc Surg. Published online June 2023:S0022522323003471. doi:10.1016/j.jtcvs.2023.04.023
- Vučurević G, Marinković S, Puškaš L, et al. Anatomy and radiology of the variations of aortic arch branches in 1,266 patients. Folia Morphol. 2013;72(2):113-122. doi:10.5603/FM.2013.0019
- Prakash null, Mokhasi V, Rajini T, Shashirekha M. The abdominal aorta and its branches: anatomical variations and clinical implications. Folia Morphol. 2011;70(4):282-286.
- Matveev DV, Kuznetsov MR, Matveev AD, Evteev AV, Fedorov EE. Reperfusion syndrome: state of the art. Angiol Vasc Surg. 2020;26(4):176. doi:10.33529/ANGIO2020421
- Pietri P, Adovasio R, Pancrazio F, Sichel L, Fazio F. Acute thrombosis of the infrarenal aorta. Therapeutic problems. Int Angiol J Int Union Angiol. 1987;6(4):397-400.
- Littooy FN, Baker WH. Acute aortic occlusion—A multifaceted catastrophe. J Vasc Surg. 1986;4(3):211-216. doi:10.1016/0741-5214(86)90187-4
- Rathore A, Gloviczki P, Oderich GS, Bower TC. Collapsed bifurcated modular infrarenal endograft. J Vasc Surg. 2019;70(2):600-605. doi:10.1016/j.jvs.2018.12.049
- Hines GL, Liu HH. Acute Aortic Occlusion and Its Sequelae: Metabolic, Pathologic Etiology, and Management. Cardiol Rev. 2021;29(2):57-61. doi:10.1097/CRD.0000000000000313
- Miroslav M, Lazar D, Aleksandar M, Predrag D, Svetozar P. Rare Forms of Peripheral Arterial Embolism: Review of 11 Cases. Vascular. 2005;13(4):222-229. doi:10.1258/rsmvasc.13.4.222
- Hussain SMA. Tumor embolism and acute arterial occlusion: A systematic review. Surgery Open Science. 2022;10:216-222. doi:10.1016/j.sopen.2022.10.006
- Dossa CD. Acute Aortic Occlusion: A 40-Year Experience. Arch Surg. 1994;129(6):603. doi:10.1001/archsurg.1994.01420300041006
- Bradbury AW, Stonebridge PA, John TG, Ruckley CV, Jenkins AMcl, Murie JA. Acute thrombosis of the non-aneurysmal abdominal aorta. Eur J Vasc Surg. 1993;7(3):320-323. doi:10.1016/S0950-821X(05)80016-7
- Crawford JD, Perrone KH, Wong VW, et al. A modern series of acute aortic occlusion. J Vasc Surg. 2014;59(4):1044-1050. doi:10.1016/j.jvs.2013.10.080
- Robinson WP, Patel RK, Columbo JA, et al. Contemporary Management of Acute Aortic Occlusion Has Evolved but Outcomes Have Not Significantly Improved. Ann Vasc Surg. 2016;34:178-186. doi:10.1016/j.avsg.2015.12.021
- Sieber S, Stoklasa K, Reutersberg B, et al. Acute abdominal aortic occlusion: A 16-year single-center experience. J Vasc Surg. 2021;74(6):1894-1903.e3. doi:10.1016/j.jvs.2021.06.021
- Bell JW. Acute Thrombosis of the Subrenal Abdominal Aorta. Arch Surg. 1967;95(4):681. doi:10.1001/archsurg.1967.01330160151023
- De Varona Frolov SR, Acosta Silva MP, Volo Pérez G, Fiuza Pérez MD. Outcomes After Treatment of Acute Aortic Occlusion. Cir Esp Engl Ed. 2015;93(9):573-579. doi:10.1016/j.cireng.2013.07.035
- Webb KH, Jacocks MA. Acute aortic occlusion. Am J Surg. 1988;155(3):405-407. doi:10.1016/S0002-9610(88)80100-4
- Drager SB, Riles TS, Imparato AM. Management of acute aortic occlusion. Am J Surg. 1979;138(2):293-295. doi:10.1016/0002-9610(79)90389-1
- Cowan KN, Lawlor DK. Sudden onset of paraplegia from acute aortic occlusion: a review of 2 cases and their unique presentation. Am J Emerg Med. 2006;24(4):479-481. doi:10.1016/j.ajem.2006.01.008
- Bloom B, Gibbons R, Brandis D, Costantino T. Point-of-care Ultrasound Diagnosis of Acute Abdominal Aortic Occlusion. Clin Pract Cases Emerg Med. 2020;4(1):79-82. doi:10.5811/cpcem.2019.11.44311
- Drake A, Dreyer N, Hoffer M, Boniface K. Point-of-care Ultrasound for the Evaluation of Acute Arterial Pathology in the Emergency Department: A Case Series. Clin Pract Cases Emerg Med. 2022;6(1):13-19. doi:10.5811/cpcem.2021.11.54904
- Björck M, Earnshaw JJ, Acosta S, et al. Editor’s Choice – European Society for Vascular Surgery (ESVS) 2020 Clinical Practice Guidelines on the Management of Acute Limb Ischaemia. Eur J Vasc Endovasc Surg. 2020;59(2):173-218. doi:10.1016/j.ejvs.2019.09.006
- Jongkind V, Earnshaw JJ, Bastos Gonçalves F, et al. Editor’s Choice – Update of the European Society for Vascular Surgery (ESVS) 2020 Clinical Practice Guidelines on the Management of Acute Limb Ischaemia in Light of the COVID-19 Pandemic, Based on a Scoping Review of the Literature. Eur J Vasc Endovasc Surg. 2022;63(1):80-89. doi:10.1016/j.ejvs.2021.08.028
- Ni YN, Wang YM, Liang BM, Liang ZA. The effect of hyperoxia on mortality in critically ill patients: a systematic review and meta analysis. BMC Pulm Med. 2019;19(1):53. doi:10.1186/s12890-019-0810-1
- Laoire ÁN, Murtagh FEM. Systematic review of pharmacological therapies for the management of ischaemic pain in patients with non-reconstructable critical limb ischaemia. BMJ Support Palliat Care. 2018;8(4):400-410. doi:10.1136/bmjspcare-2017-001359
- Mitchell AC, Fallon MT. A single infusion of intravenous ketamine improves pain relief in patients with critical limb ischaemia: results of a double blind randomised controlled trial. Pain. 2002;97(3):275-281. doi:10.1016/S0304-3959(02)00033-7
- Yee J, Kaide C. Emergency Reversal of Anticoagulation. West J Emerg Med. 2019;20(5):770-783. doi:10.5811/westjem.2018.5.38235
- Li J, Wang B, Wang Y, et al. Therapeutic effect of liposomal prostaglandin E1 in acute lower limb ischemia as an adjuvant to hybrid procedures. Exp Ther Med. 2013;5(6):1760-1764. doi:10.3892/etm.2013.1061
- De Donato G, Gussoni G, De Donato G, et al. Acute Limb Ischemia in Elderly Patients: Can Iloprost be Useful as an Adjuvant to Surgery? Results from the ILAILL Study. Eur J Vasc Endovasc Surg. 2007;34(2):194-198. doi:10.1016/j.ejvs.2007.02.002
- De Donato G, Gussoni G, De Donato G, et al. The ILAILL Study: Iloprost as Adjuvant to Surgery for Acute Ischemia of Lower Limbs: A Randomized, Placebo-Controlled, Double-Blind Study by the Italian Society for Vascular and Endovascular Surgery. Ann Surg. 2006;244(2):185-193. doi:10.1097/01.sla.0000217555.49001.ca
- Fang L, Lai Z, Qiu C, et al. Endovascular Treatment for Infrarenal Aortic Occlusion: A Systematic Review and Meta-Analysis. Ann Vasc Surg. 2020;62:432-441.e13. doi:10.1016/j.avsg.2019.05.034
- Busuttil RW, Keehn G, Milliken J, et al. Aortic Saddle Embolus: A Twenty-Year Experience. Ann Surg. 1983;197(6):698???706. doi:10.1097/00000658-198306000-00008
- Rutherford RB, Baker JD, Ernst C, et al. Recommended standards for reports dealing with lower extremity ischemia: Revised version. Journal of Vascular Surgery. 1997;26(3):517-538. doi:10.1016/S0741-5214(97)70045-4
- Brzezicki G, Machinis T, Reavey-Cantwell J. Occlusion of All Aortic Arch Great Vessels: Acute Revascularization to Perform Endovascular Stroke Therapy. World Neurosurgery. 2014;82(3-4):535.e17-535.e21. doi:10.1016/j.wneu.2013.09.019
- Tapper SS, Jenkins JM, Edwards WH, Mulherin JL, Martin RS, Edwards WH. Juxtarenal Aortic Occlusion: Annals of Surgery. 1992;215(5):443-450. doi:10.1097/00000658-199205000-00006






