Today on the emDocs cast we cover managing the high risk airway with Skyler Lentz, MD and Brit Long, MD. Part 2 covers obstructive lung disease, right heart disease, and hypoxemia.
High-Risk Airway Management Part 2
– Successful airway management is a critical skill in emergency medicine. Most emergent and unplanned intubations in the ED are managed using RSI, with success rates as high as 99%, but there are some situations that can be challenging.
– The incidence of peri-intubation cardiac arrest is as high as 1 in 25 emergency airways. Post-intubation hypotension is more common, occurring in as many as 25% of emergency intubations and is associated with increased mortality.
– Many of the pre-intubation risks for decompensation can be recognized and prevented with proper preparation and evaluation.
– Part 1 covered metabolic acidosis and shock/hypotension. Today we cover obstructive lung disease, right heart disease, and hypoxemia.
Obstructive Lung Disease

- Pitfall #1: Failure to aggressively treat with NIPPV prior to intubation.
- Pearl #1: Trial and titrate NIPPV, along with aggressive medical management, in an attempt to avoid intubation in those with obstructive lung disease.
- Pitfall #2: Not anticipating the hemodynamic risk of a high intrathoracic pressure and decreased venous return.
- Pearl #2: Ketamine may have bronchodilatory effects and is an ideal induction agent in obstructive lung disease.
- Pitfall #3: Inappropriate post intubation mechanical ventilation settings leading to breath stacking.
- Pearl #3: Use an initial ventilator strategy as shown in Table 3 and tolerate a respiratory acidosis with a pH of > 7.20.
- Pearl #4: Assess for air trapping on the ventilator. Air trapping from a high respiratory rate can lead to hemodynamic collapse; a patient with a high spontaneous respiratory rate may require deep sedation with or without neuromuscular blockade. The plateau pressure should be assessed and maintained at < 30 cm H2O.
Right Heart Disease
Pulmonary Hypertension, Right Heart Failure, and Pulmonary Embolism
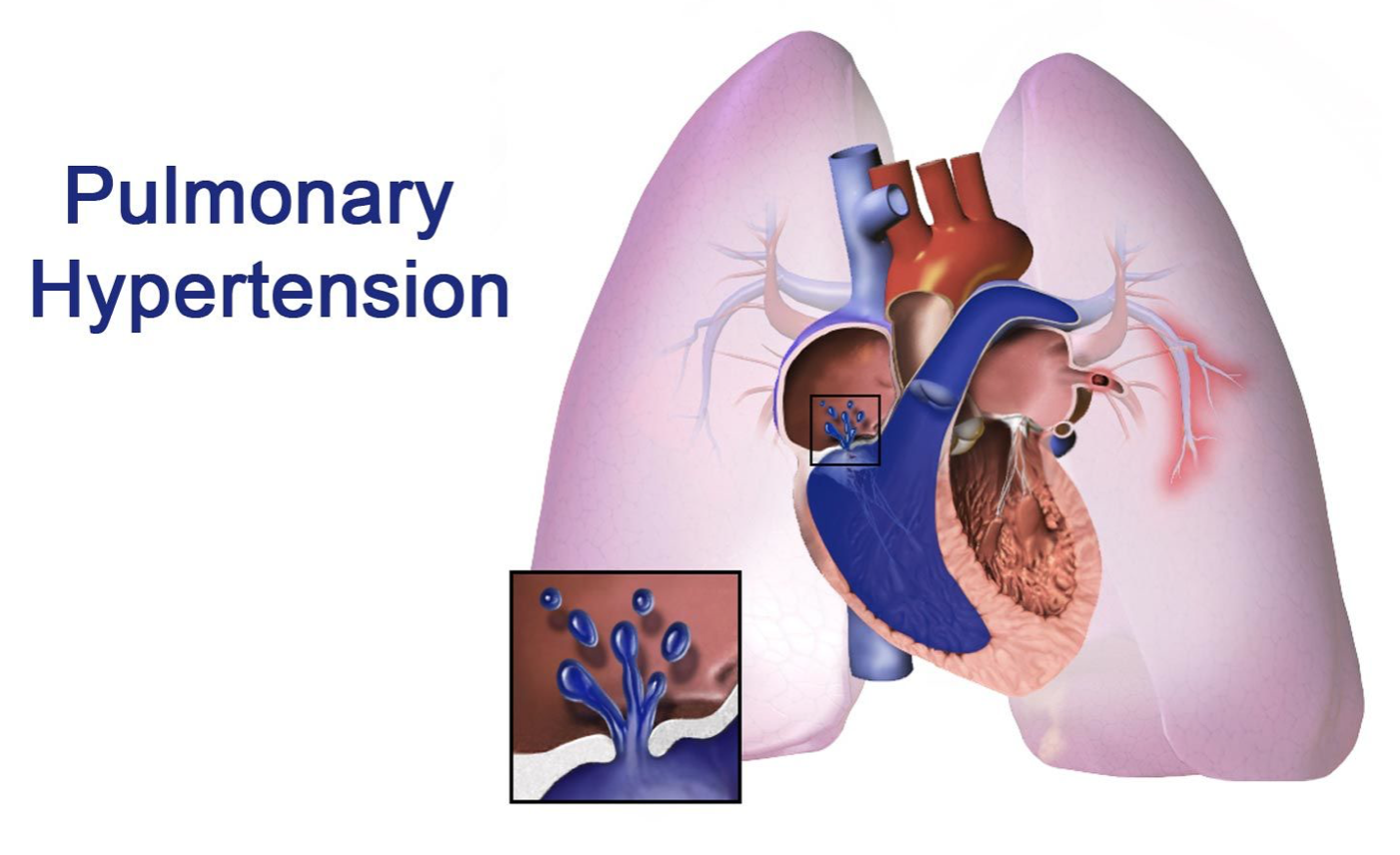
- Pitfall #1: Failure to identify a patient with pulmonary hypertension or right heart failure.
- Pearl #1: Identify those with RV failure and pulmonary hypertension using history, physical examination, and prior echocardiogram or point of care ultrasound to anticipate their complex physiology.
- Pitfall #2: Not anticipating and preparing for the hemodynamic challenges of pulmonary hypertension, right heart failure, and pulmonary embolism.
- Pearl #2: Avoid and manage precipitants of increased PVR including hypoxia, hypercapnia, and acidosis.
- Pitfall #3: Not treating hypotension, leading to an under perfused and ischemic right ventricle.
- Pearl #3: Aggressively treat systemic hypotension with norepinephrine or cautious 250-500 mL boluses only if the history suggests hypovolemia and use hemodynamically neutral induction agents. The combination of a high PA pressure and low systemic blood pressure leads to RV ischemia and risk of irreversible hemodynamic collapse.
- Pitfall #4: Inappropriate mechanical ventilation settings leading to high intrathoracic pressure post intubation.
- Pearl #4: The mechanical ventilation strategy in those with RV failure and pulmonary hypertension includes normalizing PaCO2, pH, and PaO2 with a low-pressure strategy using low PEEP (i.e. 5 cm H2O) and a low tidal volume.
- Pitfall #5: Failure to treat a pulmonary embolism prior to induction and mechanical ventilation.
- Pearl #5: In the patient with acute RV failure from PE, treatment with thrombolysis in the unstable patient prior to intubation is recommended.
- Pearl #6: Consider transfer to a specialty center for the intubated patient with known RV failure and/or pulmonary hypertension.
Severe Hypoxemia

- Pitfall #1: Failure to adequately preoxygenate prior to intubation.
- Pearl #1: Pre-intubation hypoxemia and lack of preoxygenation are predictors of adverse events.
- Pitfall #2: Not using NIPPV or appropriate positioning during preoxygenation.
- Pearl #2: Preoxygenate using NIPPV in a head-elevated position if the patient’s clinical condition allows and utilize apneic oxygenation with HFNC.
- Pitfall #3: Failure to use proper protective equipment in those with suspected respiratory infections.
- Pearl #3: Use airborne precautions when intubating and preoxygenating a patient with a highly contagious illness such as COVID-19.







