Today on the emDOCs cast with Brit Long, MD (@long_brit), we cover a deadly microangiopathic hemolytic anemia: thrombotic thrombocytopenic purpura.
Episode 45: Thrombotic Thrombocytopenic Purpura
Background
- Thrombotic thrombocytopenic purpura (TTP) is a microangiopathic hemolytic anemia.
- It is rare with 2-4 cases per million adults each year.
- Without proper management, mortality is 90%, but drops to 4% when treated correctly early.
- There is also significant morbidity with increased risks of developing chronic hypertension, lupus, and cognitive abnormalities.
Pathophysiology:
- TTP is associated with widespread microvascular thrombosis, and the central cause is a deficiency or dysfunction in ADAMTS13.
- ADAMTS13 is responsible for cleaving large von Willebrand factor pieces into smaller ones.
- TTP typically involves either a dysfunctional ADAMTS-13 or an auto-antibody against ADAMTS13.
- This results in large vWF molecules that are not cleaved, and thus they circulate as large multimers.
- These accumulate platelets and form clots, thereby using up platelets.
- There are two forms: acquired (more common in adults) vs hereditary (pediatric patients).
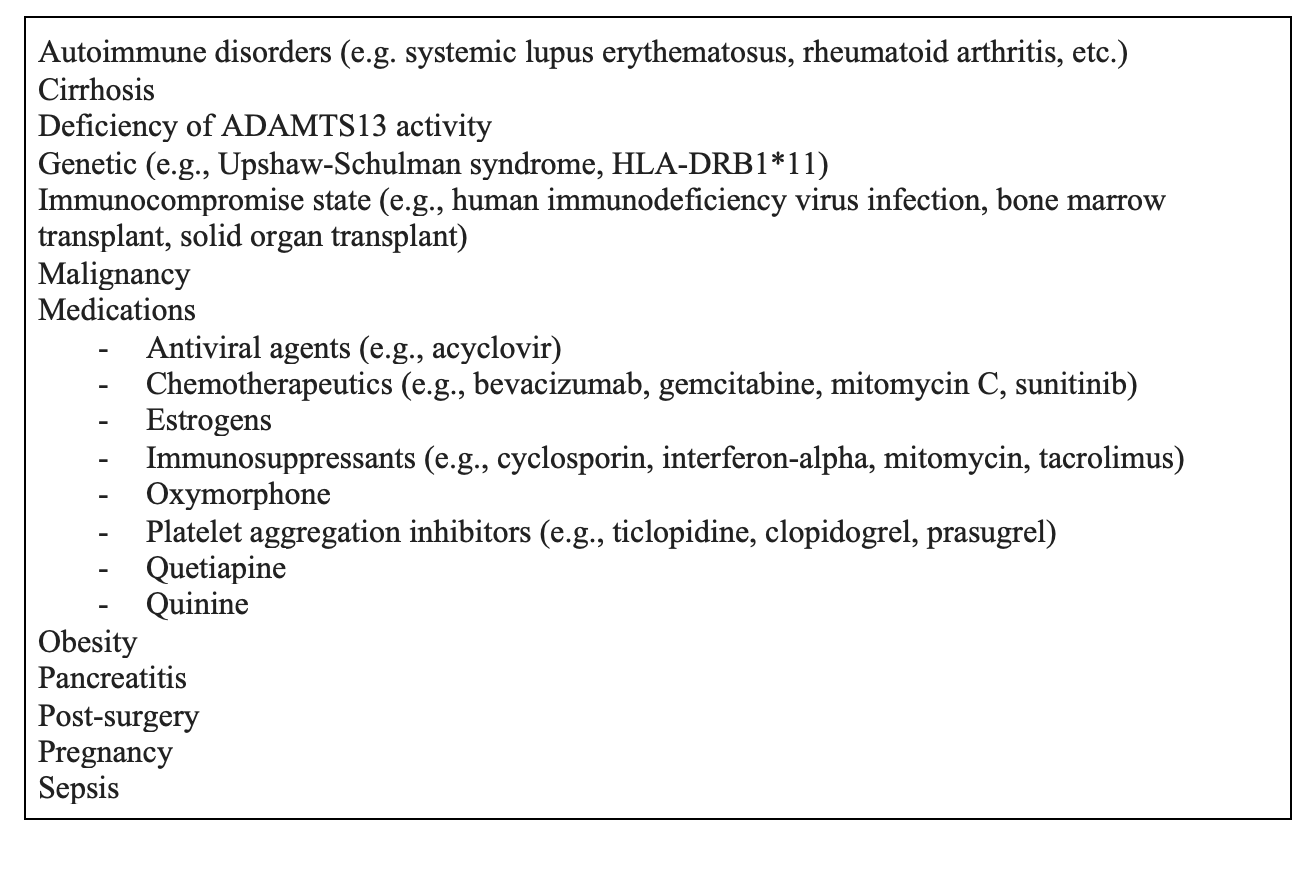
- There are a variety of triggers.
Presentation:
- Classic pentad: fever, anemia, thrombocytopenia, renal disease, neurologic dysfunction
- However, less than 7% have all five features, and many can be transient. In the ED, ask about current and recent symptoms.
- Neurologic symptoms occur in two-thirds of cases, broken into major symptoms (40%, coma, seizure, or stroke) and minor (25%, headache or transient confusion).
- Petechiae or purpura are present in half of cases, though active bleeding is rare.
- Fever is only present in about 10% of cases.
- Gastrointestinal symptoms are common; up to 70% have abdominal pain, nausea, vomiting, or diarrhea.
Evaluation:
- Laboratory analysis: anemia, thrombocytopenia, and renal injury.
- Hemoglobin is usually less than 10 with evidence of hemolysis (elevated LDH, low haptoglobin, schistocytes).
- Platelets will be less than 150, but exact number can vary.
- Renal failure is not universally present. One study found that nearly half of patients had normal renal function, while most of the remainder had a mild creatinine elevation and only 5% had renal failure.
- If possible, send an ADAMTS13 activity level and anti-ADAMTS-13 antibody test; however, this is not available in most centers.
Differentiating other diseases:
- Patients with DIC have abnormal coagulation panel and low fibrinogen (normal in TTP).
- HUS marked by severe renal disease, thrombocytopenia, high LDH, some sort of preceding illness (especially bloody diarrhea), and more common in pediatric patients.
Diagnosis:
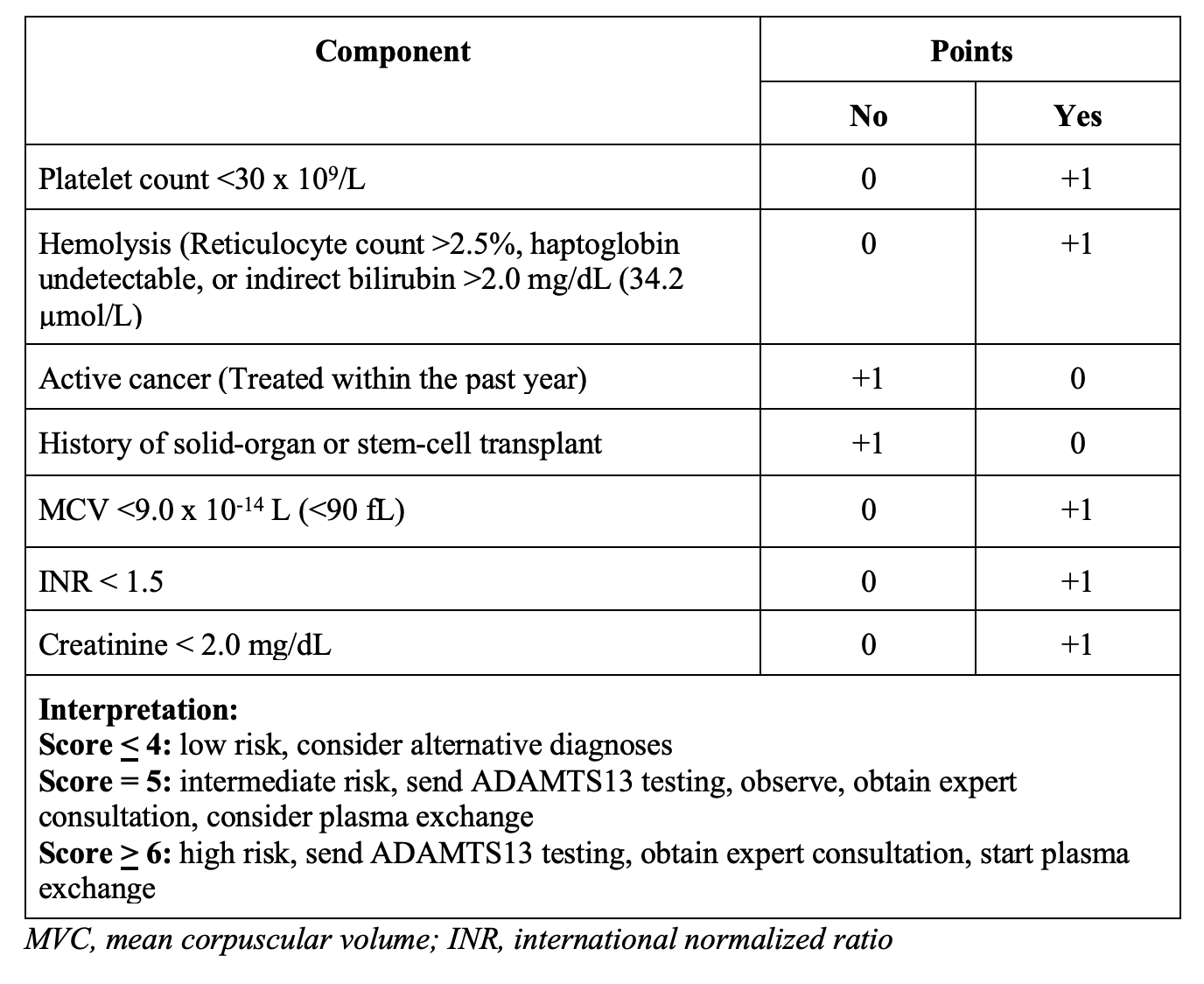
- PLASMIC score 85% sensitive and 89% specific for scores >
Management:
- Resuscitate, stabilize, treat underlying cause.
- FFP was originally used to replace the non-functioning ADAMTS13, but this is only moderately successful because auto-antibodies attack the new ADAMTS13.
- Modern therapy relies on plasma exchange and corticosteroids, which substantially reduce mortality compared with FFP alone.
- Plasma exchange removes the auto-antibodies and replaces non-functioning ADAMTS13 with functional ADAMTS13 using donor plasma.
- FFP can be administered if there will a significant delay in plasma exchange.
- Steroids reduce production of ADAMTS13 autoantibodies. Guidelines recommend methylprednisolone 1 mg/kg per day.
- Despite thrombocytopenia, active bleeding is rare and transfusions generally are not necessary.
- Platelets should not be routinely administered, but transfusion should be considered if platelets are very low and there is active bleeding or an invasive procedure is planned.
Summary:
- TTP is due to deficiency/inactivity of ADAMTS13.
- TTP is a clinical diagnosis: The classic pentad is rare; suspect TTP in a sick-appearing patient with MAHA and thrombocytopenia. Elevated LDH is also common.
- The PLASMIC score can help you with diagnosis, maybe differentiate from other conditions.
- Treatment is plasma exchange and steroids. FFP can assist if exchange is delayed.
References:
- Page EE, Kremer Hovinga JA, Terrell DR, et al. Thrombotic thrombocytopenic purpura: diagnostic criteria, clinical features, and long-term outcomes from 1995 through 2015. Blood Adv. 2017;1(10):590–600.
- Joly BS, Coppo P, Veyradier A. Thrombotic thrombocytopenic purpura. Blood. 2017;129(21):2836-2846.
- Chiasakul T, Cuker A. Clinical and laboratory diagnosis of TTP: an integrated approach. Hematology Am Soc Hematol Educ Program. 2018;2018(1):530–8.
- Blombery P, Kivivali L, Pepperell D, et al. Diagnosis and management of thrombotic thrombocytopenic purpura (TTP) in Australia: findings from the first 5 years of the Australian TTP/thrombotic microangiopathy registry. Intern Med J. 2016; 46(1):71–9.
- George JN. How I treat patients with thrombotic thrombocytopenic purpura: 2010. Blood. 2010 Nov 18;116(20):4060-9.
- George JN. Clinical practice. Thrombotic thrombocytopenic purpura. N Engl J Med. 2006 May 4;354(18):1927-35.
- Bendapudi PK, Hurwitz S, Fry A, et al. Derivation and external validation of the PLASMIC score for rapid assessment of adults with thrombotic microangiopathies: a cohort study. Lancet Haematol. 2017 Apr;4(4):e157-e164.
- Li A, Khalighi PR, Wu Q, et al. External validation of the PLASMIC score: a clinical prediction tool for thrombotic thrombocytopenic purpura diagnosis and treatment. J Thromb Haemost. 2018;16(1):164–9.
- Paydary K, Banwell E, Tong J, Chen Y, Cuker A. Diagnostic accuracy of the PLASMIC score in patients with suspected thrombotic thrombocytopenic purpura: A systematic review and meta-analysis. Transfusion. 2020 Sep;60(9):2047-2057.
- Zheng XL, Vesely SK, Cataland SR, Coppo P, Geldziler B, Iorio A, Matsumoto M, Mustafa RA, Pai M, Rock G, Russell L, Tarawneh R, Valdes J, Peyvandi F. ISTH guidelines for the diagnosis of thrombotic thrombocytopenic purpura. J Thromb Haemost. 2020 Oct;18(10):2486-2495.
- Coppo P, Schwarzinger M, Buffet M, et al; French Reference Center for Thrombotic Microangiopathies. Predictive features of severe acquired ADAMTS13 deficiency in idiopathic thrombotic microangiopathies: the French TMA reference center experience. PLoS One. 2010 Apr 23;5(4):e10208.
- Zheng XL, Vesely SK, Cataland SR, et al. ISTH guidelines for treatment of thrombotic thrombocytopenic purpura. J Thromb Haemost. 2020 Oct;18(10):2496-2502
- Sayani FA, Abrams CS. How I treat refractory thrombotic thrombocytopenic purpura [published correction appears in Blood. 2017 Oct 5;130(14 ):1684]. Blood. 2015;125(25):3860-3867.
- Blombery P, Scully M. Management of thrombotic thrombocytopenic purpura: current perspectives. J Blood Med. 2014;5:15-23.
- Fontana S, Kremer Hovinga JA, Lämmle B, Mansouri Taleghani B. Treatment of thrombotic thrombocytopenic purpura. Vox Sang. 2006 May;90(4):245-54.
- Sarode R, Bandarenko N, Brecher ME, et al. Thrombotic thrombocytopenic purpura: 2012 American Society for Apheresis (ASFA) consensus conference on classification, diagnosis, management, and future research. J Clin Apher. 2014 Jun;29(3):148-67.
- Froissart A, Buffet M, Veyradier A, et al; French Thrombotic Microangiopathies Reference Center. Efficacy and safety of first-line rituximab in severe, acquired thrombotic thrombocytopenic purpura with a suboptimal response to plasma exchange. Experience of the French Thrombotic Microangiopathies Reference Center. Crit Care Med. 2012 Jan;40(1):104-11.







