Author: Ashley Werbin, DO (Transition Year Resident, San Antonio, TX) // Edited by: Alex Koyfman, MD (@EMHighAK) and Brit Long, MD (@long_brit)
The views expressed are those of the authors and do not reflect the official views or policy of the Department of Defense or its Components.
Case
A 60-year-old male with a past medical history of hypertension presents to the emergency department (ED) with a chief complaint of severe epigastric pain. The patient looks to be in extreme discomfort, doubled over on the stretcher. The patient’s wife reports that her husband’s symptoms began about one hour after dinner. Review of systems is remarkable for bloating, nausea, and vomiting, but the patient denies radiation of pain and diarrhea/constipation. He denies ever experiencing pain like this current episode. Vital signs include Temp 99°F, BP 164/94, HR 90, RR 16, SpO2 97% RA.
Unsure of the etiology of your patient’s pain, the acute onset of his symptoms has you concerned. So, you begin to brainstorm the possibilities with particular attention paid to acute abdominal processes.
Epidemiology of Gastric Volvulus
Gastric volvulus is a relatively uncommon diagnosis, with about 80-90% of cases occurring in adults and 10-20% in children, with an equal incidence among males and females.1,2,3,4 Though unusual in adults younger than fifty years of age, those cases that do occur in children have been attributed to congenital diaphragmatic defects.1
While rare in its incidence, certain risk factors such as age greater than fifty years, phrenic nerve paralysis, stomach or splenic abnormalities, diaphragmatic irregularities, kyphoscoliosis, and diaphragmatic eventration increase the likelihood and possibility of the occurrence of gastric volvulus.2
Pathophysiology
Gastric volvulus, as the name suggests, involves the rotation (or revolution) of the stomach about an axis. Like other organs within the abdomen and peritoneum, the stomach remains in a position of anatomic normalcy via the help of four different ligaments. The gastrophrenic ligament, gastrosplenic ligament, gastrohepatic ligament, and gastrocolic ligament serve to anchor the stomach to the diaphragm, spleen, liver, and colon, respectively.2
Gastric volvulus can occur idiopathically or secondary to some other cause. Those occurring idiopathically are generally due to abnormalities of the above gastric ligaments, leading to mobility of the stomach. Examples of causes that can lead to loosening of the gastric ligaments include mass effect from malignancy, adhesions from prior surgeries, or skeletal deformities that displace the abdominal organs producing tension and elongation of the ligaments over time.2 Patients presenting with an idiopathic type gastric volvulus will complain of chronic symptoms due to the progressive slackening of these ligaments. Secondary volvulus is the result of some other anatomic abnormality causing the stomach to rotate. The most common cause of secondary volvulus is diaphragmatic defects, with paraesophageal hernia being the most common.2
The diagnosis of gastric volvulus is further classified based on the axis with which the stomach rotates, and there are two: organoaxial and mesenteroaxial.1,4
The organoaxial axis is a longitudinal axis that traverses the gastroesophageal junction and the pylorus, while the mesenteroaxial axis is a transverse axis that intersects the greater and lesser curvatures of the stomach.1,3,4 With organoaxial rotation, the antrum rotates anterosuperiorly and the fundus rotates posterioinferiorly, leading to an inverted position.2 Mesenteroaxial rotation, however, displaces the antrum above the gastroesophageal junction.2 A diagnosis of gastric volvulus requires a rotation of the stomach greater than 180°. Those involving the organoaxial axis are more likely to achieve this degree of rotation, with mesenteroaxial rotation usually only partial.4
Presenting Signs and Symptoms
As expected, the signs and symptoms of gastric volvulus involve some degree of abdominal pain. Gastric volvulus can present acutely or chronically with the following signs and symptoms: abdominal pain, chest pain, vomiting, dysphagia, bloating/distention, or indigestion. Borchardt’s Triad is present in about 70% of acute gastric volvulus cases, which includes pain, vomiting, and the inability to pass a nasogastric (NG) tube.3
Differential Diagnosis
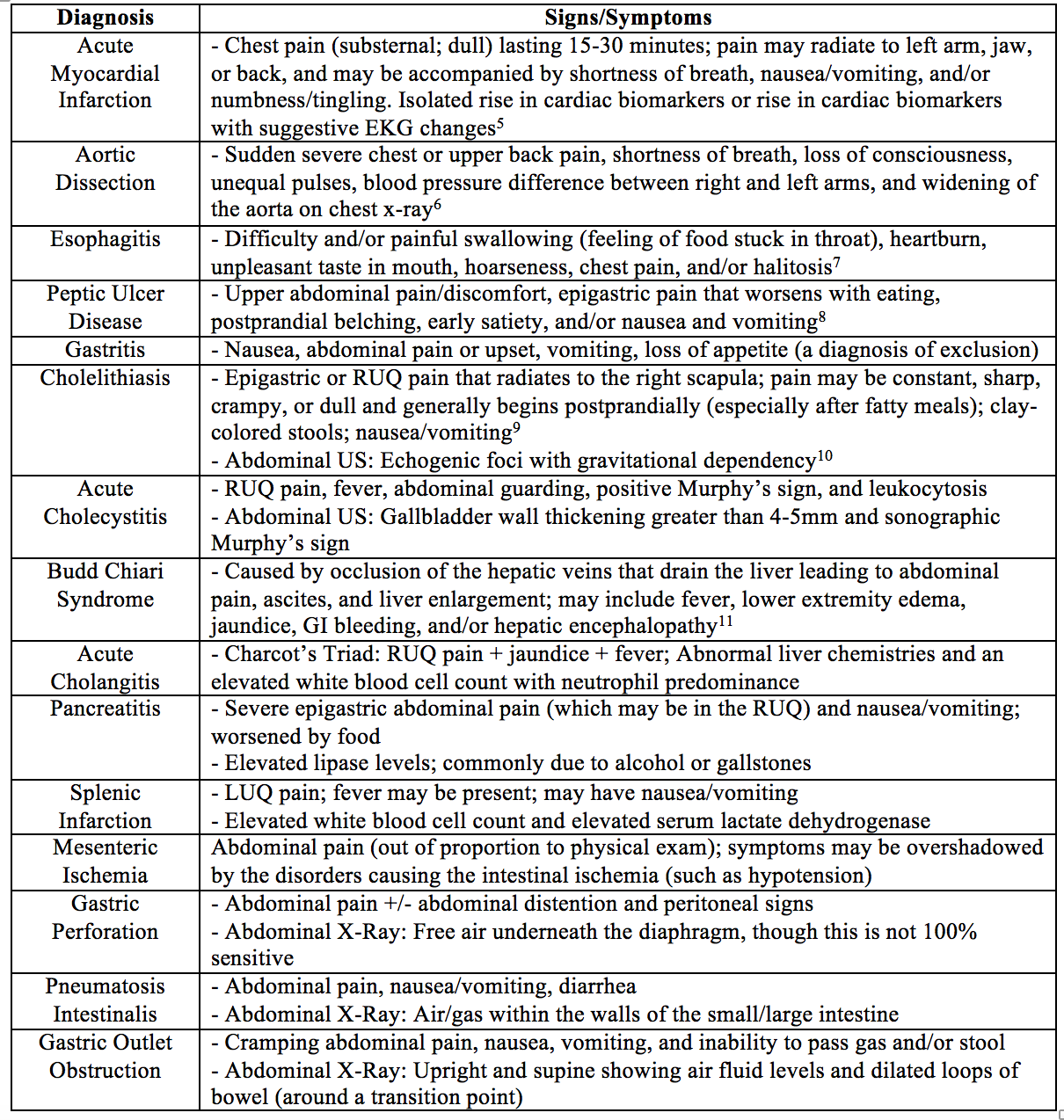
The symptoms of gastric volvulus are non-specific; hence, the emergency physician must maintain a broad differential. Below is a table of diagnoses to consider when encountering the patient with undifferentiated abdominal/epigastric pain.
Diagnosis and Treatment
The diagnosis of gastric volvulus is largely dependent on the patient’s clinical history and radiologic studies. According to the Oesophagogastric Surgery textbook, the best initial radiologic study is a chest x-ray. If diagnostic, the chest x-ray will show a “retrocardiac air fluid level and an air fluid level below [the level of] the diaphragm.”4 If the chest x-ray is inconclusive, the most definitive study is the barium swallow, which will show an obstruction at the level of the torsion.4 While the barium swallow is highly sensitive and specific for diagnosing gastric volvulus, it is important to consider what additional information could be gained if a CT scan with oral contrast is conducted. If a CT scan with oral contrast is completed, the stomach should be seen in the chest cavity, and contrast will not be visible below the diaphragm. The benefit of a CT scan over a barium swallow is the ability to see other abdominal organs and structures and their spatial relationship to the stomach, which is especially helpful in determining if the gastric volvulus is of primary or secondary origin. The radiographic appearance of a diagnosis of gastric volvulus on chest x-ray, barium swallow, and CT scan are exemplified at Radiopaedia.
Acute gastric volvulus is a surgical emergency associated with significant morbidity and mortality if not diagnosed quickly.15 Upon diagnosis of gastric volvulus, the first step in treatment is stabilizing the patient. IV fluids, analgesics, and antiemetics are essential. Adjuncts to this step include providing IV fluids and decompressing the stomach by inserting an NG tube and attaching it to suction. The NG must be placed carefully to avoid perforation, especially in the pediatric patient. If the placement of the NG tube is successful, surgery does not have to occur emergently. On the other hand, if unable to place an NG tube, the patient must undergo emergent decompression and derotation, and there are two ways to achieve this.2
Surgical management of acute gastric volvulus can be accomplished in two ways: endoscopic derotation with percutaneous endoscopic gastrostomy tube (PEG tube) placement or laparotomy. Endoscopic derotation and PEG tube placement involves manipulating/derotating the stomach with an endoscope and placement of two PEG tubes (in the gastric body and distal stomach) for several weeks to stimulate scar formation.2 The goals of open surgery include: derotation of the volvulus, debridement of non-viable tissue (consequence of ischemia), reduction and closure of the hernia (if the volvulus is deemed to have been caused by a diaphragmatic defect), and gastropexy (or surgical fixation of the stomach) to prevent recurrence.4
The Emergency Department Approach
Abdominal pain with or without nausea and vomiting characterizes a wide range of disorders. When addressing the patient presenting to the ED with these complaints, the emergency physician should always:
- Assess the patient’s airway, breathing, and circulatory status intervening when necessary, while obtaining your safety net of bilateral IV’s, O2, monitors, and pulse oximetry
- Resuscitate with IV fluids and antimicrobials if the patient meets SIRS criteria and infection is suspected
- Perform a thorough history regarding medical comorbidities, previous surgeries, and the onset and duration of symptoms
- Perform a focused physical exam paying particular attention to heart sounds, the presence of abdominal distention, dullness to percussion over the gastric area, and/or lack of bowel sounds
- Evaluate for cardiac etiology via EKG and serum cardiac biomarkers
- Utilize the history and physical, as well as other ancillary studies (chest x-ray) to make educated decisions regarding further evaluation, treatment, and disposition
Key Points
- Perform a thorough history and physical exam by first addressing the stability of the patient’s condition (airway, breathing, circulatory status)
- Obtain an EKG and serum cardiac biomarkers to rule out cardiac etiology in those patients presenting with undifferentiated epigastric pain
- Order a chest x-ray
- If chest x-ray reveals air fluid levels above and below the diaphragm, administer IV fluids and insert nasogastric tube
- Successful placement => non-emergent surgery
- Unsuccessful placement => emergent surgery
- If chest x-ray is inconclusive, consider CT scan with oral contrast or emergent barium swallow study
- If chest x-ray reveals air fluid levels above and below the diaphragm, administer IV fluids and insert nasogastric tube
This post is sponsored by www.ERdocFinder.com, a supporter of FOAM and medical education, who with their sponsorship are making FOAM material more accessible to emergency physicians around the world.
References / Further Reading:
- Hope, W. and Geibel, J. Gastric Volvulus. Medscape. 2017. Available from http://emedicine.medscape.com/article/2054271-overview#a3.
- Wee, J.O., Soybel, D.I. and Wenliang, C. Gastric volvulus in adults. Up to Date. July 2017. Available from https://www.uptodate.com/contents/gastric-volvulus-in-adults?source=search_result&search=gastric%20volvulus&selectedTitle=1~14.
- Wani, B.N. and Jajoo, S. Gastric volvulus. Indian Journal of Surgery. 2010; 72:163-164. DOI: 10.1007/s12262-010-0039-y.
- Bronson, N.W., Perry, K.A. and Hunter, J.G. Paraoesophageal hernia and gastric volvulus. In: Oesophagogastric Surgery. 5th Saunders Elsevier, 2014:308-316.
- Reeder, G.S. and Kennedy, H.L. Criteria for the diagnosis of acute myocardial infarction. Up to Date. July 2016. Available from https://www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-myocardial-infarction?source=search_result&search=acute%20myocardial%20infarction&selectedTitle=2~150.
- Diseases and Conditions Aortic Dissection. Mayo Clinic. 2014. Available from http://www.mayoclinic.org/diseases-conditions/aortic-dissection/basics/definition/con-20032930.
- Cunha, J.P. Esophagitis. E-Medicine Health. 2016. Available from http://www.emedicinehealth.com/esophagitis/page2_em.htm.
- Vakil, N.B. Peptic ulcer disease: Clinical manifestations and diagnosis. Up to Date. 2015. Available from https://www.uptodate.com/contents/peptic-ulcer-disease-clinical-manifestations-and-diagnosis?source=search_result&search=peptic%20ulcer%20disease&selectedTitle=2~150.
- Vorvick, L.J. Gallstones. The New York Times Health Guide. 2011. Available from http://www.nytimes.com/health/guides/disease/gallstones/overview.html#Symptoms.
- Afdhal, N.H. Approach to the patient with incidental gallstones. Up to Date. 2016. Available from https://www.uptodate.com/contents/approach-to-the-patient-with-incidental-gallstones?source=search_result&search=cholelithiasis&selectedTitle=1~150.
- Lai, M. Budd-Chiari syndrome: Epidemiology, clinical manifestations, and diagnosis. Up to Date. 2017. Available from https://www.uptodate.com/contents/budd-chiari-syndrome-epidemiology-clinical-manifestations-anddiagnosis?source=search_result&search=budd%20chiari%20syndrome&selectedTitle=1~125#H79562169.
- Images provided courtesy of Radswiki, Radiopaedia.org, rID: 11448.
- Images provided courtesy of Dr. Amro Omar, Radiopaedia.org, rID: 19805.
- Images provided courtesy of Dr. Maxime St-Amant, Radiopaedia.org, rID: 19257.
- Gerstle, J.T., Chiu, P. and Emil, S. Gastric volvulus in children: lessons learned from delayed diagnoses. Seminars in Pediatric Surgery. 2009; 18(2):98-103.







