Journal Feed Weekly Wrap-Up
- Jul 11th, 2020
- Clay Smith
- categories:
We always work hard, but we may not have time to read through a bunch of journals. It’s time to learn smarter.
Originally published at JournalFeed, a site that provides daily or weekly literature updates.
Follow Dr. Clay Smith at @spoonfedEM, and sign up for email updates here.
#1: HALT-IT – TXA for GI Bleed
Spoon Feed
TXA did not reduce mortality within 5 days in patients with upper or lower GI bleeding, but it did increase risk of venous thromboembolism.
Why does this matter?
TXA reduces risk of death from traumatic hemorrhage. Might it also work for GI bleeding?
HALT-IT…or not
This was a large, multi-center randomized, double-blinded, placebo controlled trial of 12,009 patients with upper or lower GI bleeding comparing TXA vs placebo/usual care. For the primary outcome of mortality within 5 days, there was no difference; both had 4% mortality. There was no increase in arterial thrombotic events but nearly double the risk of venous thromboembolism in the TXA group (0.8% TXA vs 0.4% placebo; RR 1·85, 95%CI 1.15 to 2.98). Some interventions help GI bleeds, just not TXA.
Source
Effects of a high-dose 24-h infusion of tranexamic acid on death and thromboembolic events in patients with acute gastrointestinal bleeding (HALT-IT): an international randomised, double-blind, placebo-controlled trial. Lancet. 2020 Jun 20;395(10241):1927-1936. doi: 10.1016/S0140-6736(20)30848-5.
Open in Read by QxMD
#2: Silent Hypoxemia from COVID-19 Explained
Spoon Feed
The severe, yet clinically silent hypoxemia of COVID-19 seen in some patients may be explained by a few basic respiratory pathophysiological principles.
Why does this matter?
Dubbed “happy hypoxia,” the silent hypoxemia of COVID-19 has caused consternation among seasoned physicians. Rich Levitan remarked in a NYT op-ed that patients had profound hypoxia, “seemingly incompatible with life—but they were using their cellphones…” The authors offer some possible explanations for this phenomenon.
There’s nothing happy about hypoxia
The authors present three cases, all with COVID-19, minimal respiratory distress, yet profound hypoxemia. How can this be? The authors pose seven possible explanations.
-
Hypoxia alone does not trigger a large increase in minute ventilation until the PaO2 has dropped below 60; below that, it increases exponentially. See Figure 1.
-
Ventilatory drive is profoundly influenced by PCO2. “Severe hypoxia elicits an effective increase in ventilation only when background PaCO2 exceeds 39 mmHg.”
-
Increasing age and diabetes may decrease the responsiveness of the respiratory drive in response to hypoxia. Also, individuals vary widely in their sensitivity to the O2 and CO2 triggers of respiratory drive.
-
Pulse oximeters are notoriously inaccurate below 80%. SpO2 is also less accurate in critically ill patients and Black patients. See Figure 2.
-
Of course, profoundly low oxygen levels are deleterious for even a brief period of time, but humans can tolerate fairly low PaO2 for extended periods of time and may not feel bad. The authors remind us that tourists driving on Mt. Evans in Colorado routinely have a drop in SpO2 to 65%, and many feel no sense of dyspnea.
-
Fever shifts the oxyhemoglobin dissociation curve right, meaning a lower SaO2 for the same PaO2. The carotid body only senses PaO2.
-
They also remind us that hypoxemia must be defined in relation to the FiO2. Is a patient on 100% FiO2 with SpO2 92% hypoxic? Most physicians surveyed for this commentary would say yes. The authors comment that it may be difficult to judge severity based on number of liters of oxygen, given that it can be difficult to know the true FiO2 in non-intubated cases.
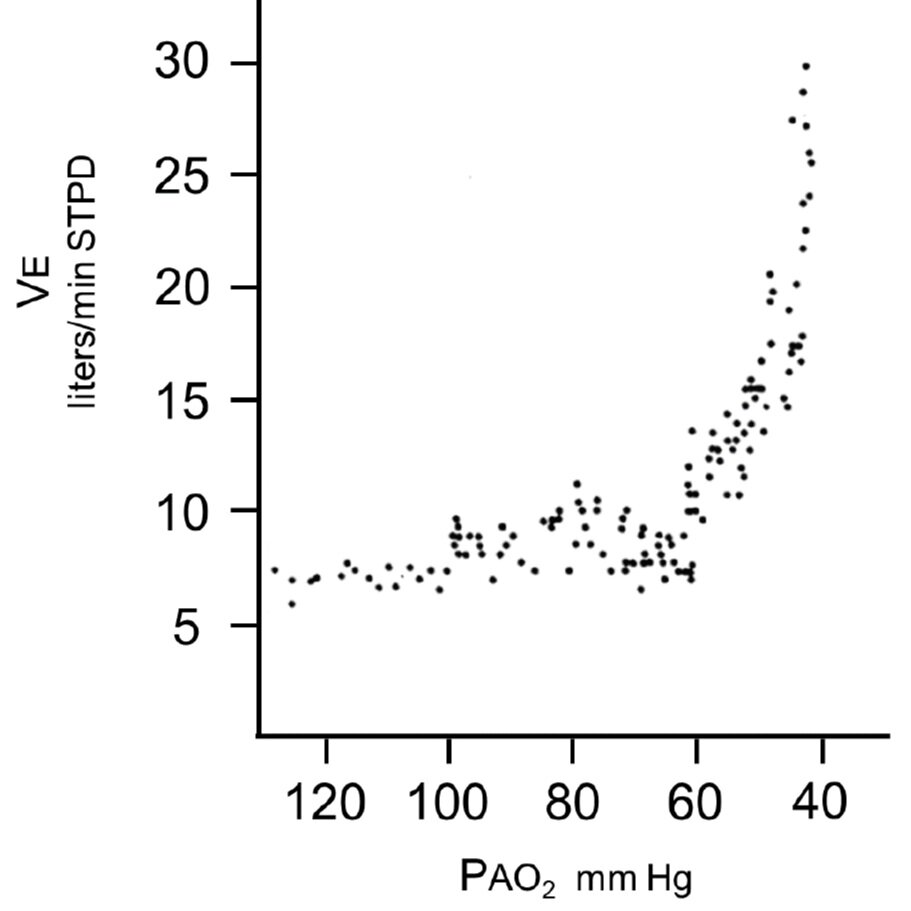
From cited article – Figure 1. PaO2 <60 marked increase minute ventilation
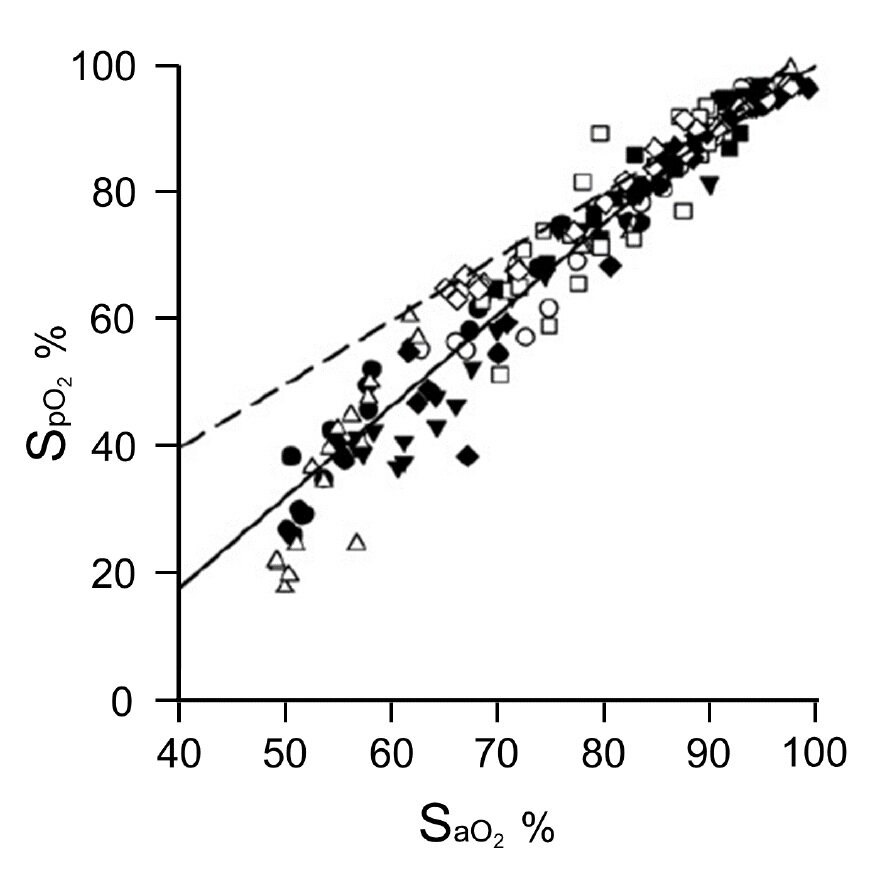
From cited article – Figure 2. Below 80%, SpO2 underestimates SaO2.
Source
Why COVID-19 Silent Hypoxemia is Baffling to Physicians. Am J Respir Crit Care Med. 2020 Jun 15. doi: 10.1164/rccm.202006-2157CP. [Epub ahead of print]
Open in Read by QxMD
#3: Does Syncope in PE Mean Increased Mortality?
Spoon Feed
PE with syncope is associated with increased risk of short-term mortality, which is explained by the increase in hemodynamic instability seen in these patients as well.
Why does this matter?
PESIT raised concern that 1 in 6 patients admitted with syncope had PE. Subsequently, the rate has been shown to be significantly less than that. But when a patient has a PE + syncope, does that portend a bad outcome?
Not all syncope is PE, but PE with syncope is bad.
This was a meta-analysis of 20 studies, pooling 9,419 patients. They found that when a patient had syncope associated with PE, the odds of short-term mortality increased 82% (OR 1.82, 95%CI 1.14 to 2.90). Odds of hemodynamic instability was also much greater in patients with syncope (OR 4.36, 95%CI 2.27 to 8.37). In fact, the increased risk of mortality in patients with PE + syncope was explained by the increase in hemodynamic instability. The authors point out that this is why it is important to use hemodynamic status to risk stratify patients who present with PE and syncope.
Source
The Prognostic Value of Syncope on Mortality in Patients With Pulmonary Embolism: A Systematic Review and Meta-analysis. Ann Emerg Med. 2020 May 24. pii: S0196-0644(20)30216-X. doi: 10.1016/j.annemergmed.2020.03.026. [Epub ahead of print]
Open in Read by QxMD
