Journal Feed Weekly Wrap-Up
- Jul 10th, 2021
- Clay Smith
- categories:
#1: Anterior ST Elevation: MI or Early Repolarization?
Spoon Feed
When ST elevation is present in the anterior precordial leads, a validated 4-variable formula can help differentiate LAD coronary occlusion from benign early repolarization.
Why does this matter?
ST elevation in the anterior precordial leads can be tricky. In some cases, it represents acute myocardial infarction, and in other cases it represents a benign finding. This distinction will drastically change the patient’s plan of care, so we must be sure we can spot the difference. While abnormal R wave progression or abnormal ST segment morphology may provide some subtle clues for acute ischemia, wouldn’t it be great if there were a validated method for determining the difference?
Bad news or benign finding?
This Annals clinical case features an ECG with ST segment elevation in the anterior precordial leads, similar to the open access example below (from Dr. Smith’s ECG blog, licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, ECG not modified). While the Annals ECG doesn’t meet STEMI criteria for cath lab activation, it does have subtle changes to suggest occlusion myocardial infarction of the LAD as opposed to benign early repolarization. R-wave regression and a straight ST segment morphology provide convincing clues in the Annals article. The ECG below has minimal ST elevation in V1-V4. Is there another way to be more sure this subtle anterior ST elevation is truly concerning before you call cardiology?
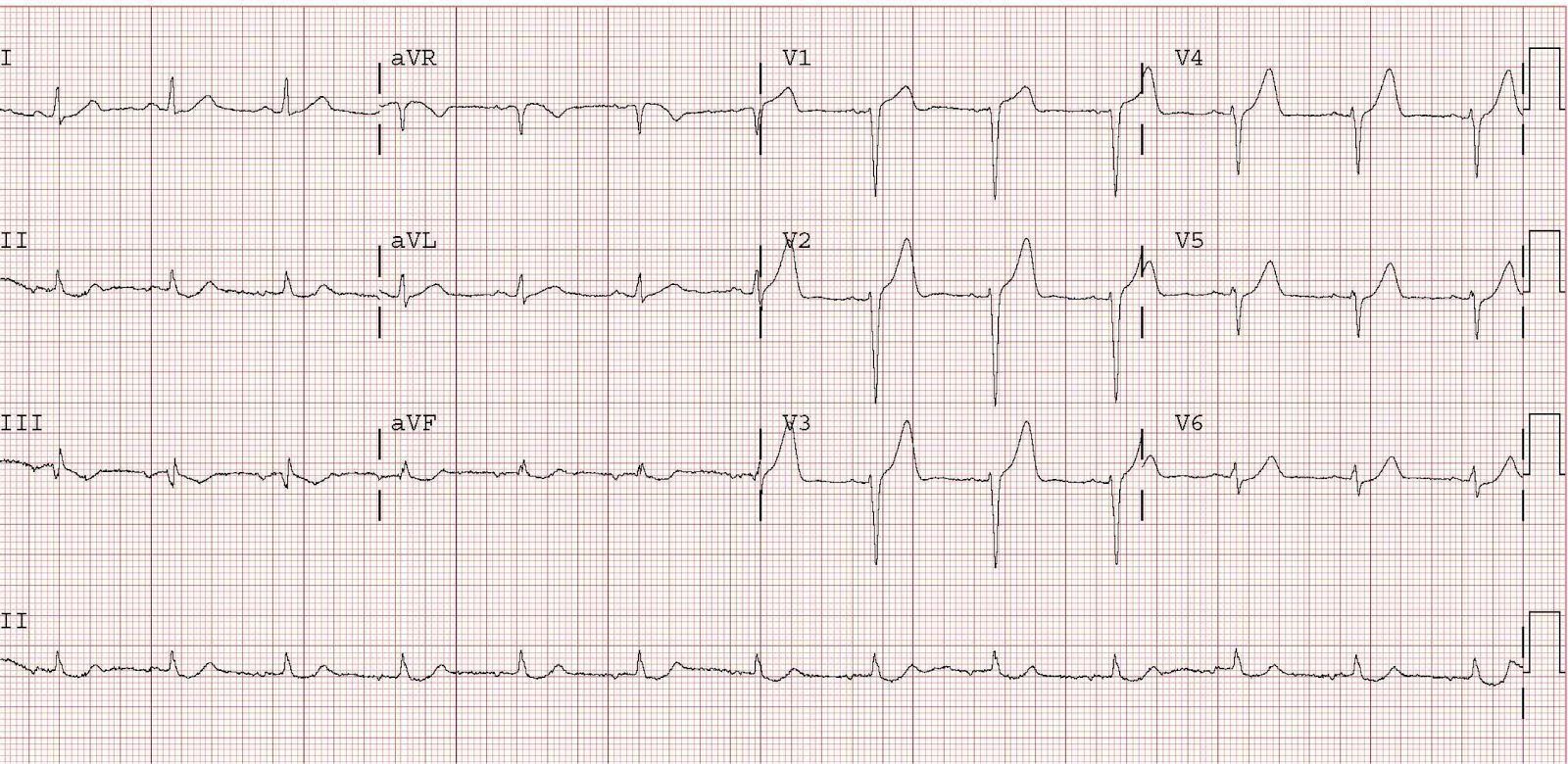
This is from Dr. Smith’s ECG blog and is not the ECG from the cited article, though it illustrates the same point. This tracing is a 46 year old with chest pain. It does not have R-wave regression, but it does have poor R wave progression. Click image for source link.
A validated formula exists to help with this differentiation, and while it’s not something that can be easily memorized, it can be readily found and utilized through online resources like MDCalc. You’ll need to calculate the QTcB, QRS amplitude in V2, R wave amplitude in V4, and the ST segment elevation 60ms after the J point in V3, and input these numbers into the formula. The calculator does the hard work and provides a number that predicts with high sensitivity and specificity whether or not you have an occlusion myocardial infarction. I encourage you to try this out next time you’re on the fence about an ECG with some anterior precordial ST segment elevation of unclear significance. In fact, click the MDCalc link and try it on the ECG above. What does the 4-variable calculator show with this tracing: likely benign early repolarization or likely anterior STEMI? If you have the chance to read this one in full text, the ECG examples are worth a look.
Source
Anterior ST Elevation: Early Repolarization or Occlusion Myocardial Infarction? Ann Emerg Med. 2021 Jun;77(6):593-596. doi: 10.1016/j.annemergmed.2020.09.443.
#2: How to Manage Postpartum Hemorrhage
Spoon Feed
Postpartum hemorrhage is defined as ≥1000mL of blood loss irrespective of the delivery route, with associated shock. Remember the four “T’s”: tone (uterine atony), trauma (lacerations, uterine rupture), tissue (retained placenta, clots) and thrombin (coagulopathies). Manage the ABCs (especially two large bore IV’s for massive transfusion) and tailor treatment to the specific cause. Recommendations for balanced transfusion are derived from the trauma literature, but it is important to administer cryoprecipitate earlier to maintain a higher fibrinogen level (at term the normal level is >350mg/dL). See Table 2 for blood product replacement recommendations.
Why does this matter?
Due to increased blood flow to the uterus during pregnancy (~600mL/min as opposed to the normal 60mL/min), postpartum hemorrhage remains the leading cause of maternal illness and death globally. Rapid intervention by treating the common causes of postpartum hemorrhage and associated hemorrhagic shock can be life-saving. Anticipating those patients who are at higher risk for postpartum hemorrhage can allow for earlier mobilization of resources and intervention. Risk factors include: prior c-section, multiple gestation, >4 prior vaginal deliveries, large fibroids, baseline low hemoglobin or coagulopathy, abnormal placentation, and more in Table 3. As you can see, this is an important article you will want to read in full text. If not a subscriber, you can read two free articles per month on the NEJM website. This should probably be one of them.
Spill the TTTTea…tone, trauma, tissue and thrombin
-
Tone (the most common cause of postpartum hemorrhage)
-
Risk factors: chorioamnionitis, therapeutic use of magnesium sulfate, prolonged or precipitous delivery, induction of labor or augmentation of labor, uterine fibroids, fetal macrosomia or polyhydramnios, caesarean sections, advanced maternal age and extremes of parity
-
Management of uterine atony:
-
1st: perform bimanual uterine massage in order to induce uterine contraction by stimulating endogenous prostaglandin release
-
2nd: treat with medications (You’ll want to check out Table 1 for a review on mechanism of action, route/dose, side effects and contraindications.)
-
1st line: Oxytocin
-
2nd line: methylergonovine maleate (Methergine) and carboprost tromethamine (Hemabate)
-
Adjunctive agents: tranexamic acid (TXA) and recombinant factor VIIa
-
-
3rd: mechanical compression via uterine compression sutures (brace sutures) or balloon tamponade systems (Bakri balloon, Figure 2)
-
4th: If all other methods have failed, surgical methods via bilateral uterine artery ligation, internal iliac artery ligation or hysterectomy can be life-saving.
-
-
Management of uterine inversion: immediate manual replacement (tocolytic agents may be required to relax the uterus)
-
-
Trauma
-
Risk factors: operative vaginal delivery, precipitous delivery and episiotomy
-
Management of genital tract lacerations: careful inspection for cervical, vaginal, perineal and rectovaginal lacerations followed by prompt repair with absorbable sutures
-
-
Tissue
-
Risk factors: incomplete delivery of placenta, placenta accreta spectrum
-
Management of retained placental tissue: evacuation of retained products either manually or with the use of a curette under ultrasound guidance
-
-
Thrombin
-
Risk factors: pre-eclampsia, HELLP syndrome, intrauterine fetal death, placental abruption, acquired coagulopathy (amniotic fluid embolism) and inherited coagulopathy
-
Management: correct coagulopathy while providing hemodynamic support and delivering the fetus
-
Source
Postpartum Hemorrhage. N Engl J Med. 2021 Apr 29;384(17):1635-1645. doi: 10.1056/NEJMra1513247.
Spoon Feed
In patients that develop febrile neutropenia, procalcitonin (PCT) levels were better at identifying those at a higher risk for 30-day mortality and bacteremia than the commonly used MASCC score.
Why does this matter?
Febrile neutropenia is a common complication of chemotherapy. Neutropenia is defined as an absolute neutrophil count (ANC) <1500 or 1000 cells/mL, depending on the institution, with severe neutropenia defined as an ANC <500 cells/mL. The Infectious Diseases Society of America defines fever in neutropenic patients as a single oral temperature of >38.3 degrees Celsius or a temperature of >38.0 degrees Celsius sustained over one hour. Identifying those patients that are at low-risk for potential complications of febrile neutropenia who could be safely managed as an outpatient would reduce the burden of hospital admission and eliminate the risk of exposure to nosocomial infections.
I love SoCal, I mean ProCal
100 patients were included in this prospective, observational study to determine 30-day mortality using MASCC score and subsequent PCT levels. Of these 100 patients, 92 had hematologic malignancies and 8 had solid tumors. All patients had an ANC <1000 and a single fever of >38 degrees Celsius. During evaluation in the emergency department, a MASCC score was assigned to each patient, and then blood cultures and a point-of-care PCT were drawn prior to starting antibiotics. Of the 100 patients, 54 were classified as low-risk by MASCC score (≥21). The median value of PCT in patients deemed low-risk (MASCC ≥ 21) was 0.735 ng/mL and with MASCC scores <21 was 1.48 (lower MASCC scores mean greater risk). When PCT levels were drawn in the low risk patient group (N=54), 19 patients had PCT levels above 1.42. Of these 19 patients, 9 died within 30 days. The PCT cutoff value was determined to be 1.42 ng/mL to yield an AUROC of 0.66, which demonstrated higher sensitivity, specificity, PPV and NPV for mortality and bacteremia than MASCC scores. See Table.
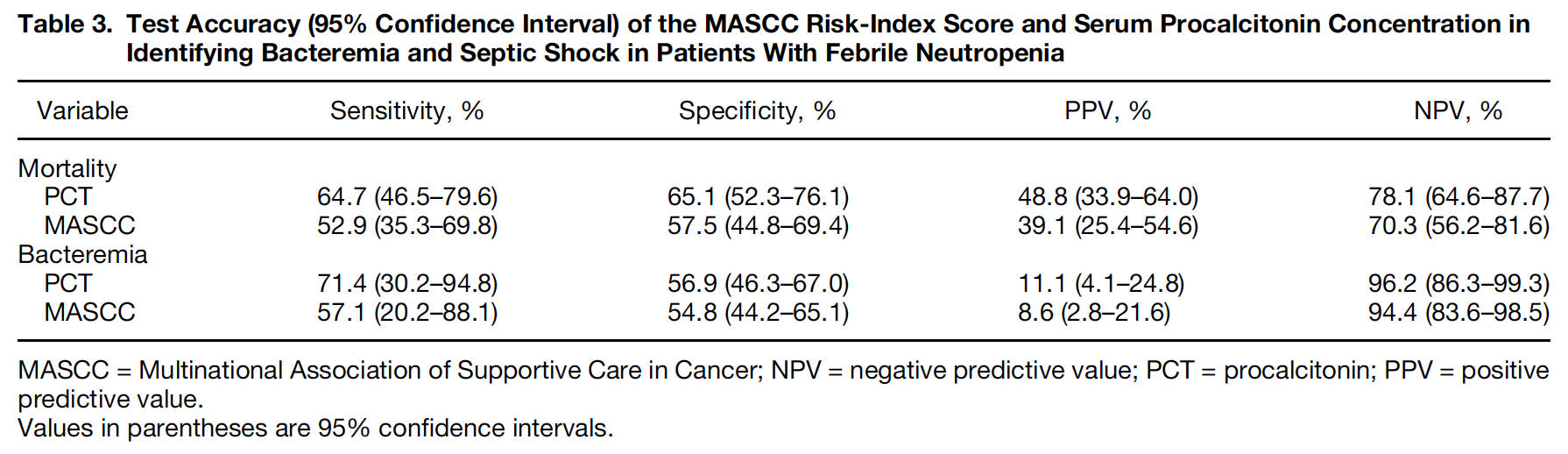
From cited article
I certainly think procalcitonin can be used in the emergency department as an objective data point to aid in the decision to admit or discharge and would remove the subjective component of the MASCC score; however, it is important to note that the study population was relatively young (mean age 30.2), predominantly male (70%), and biased towards hematologic malignancies (92%).
Editor’s note: Neither MASCC nor PCT is a great discriminator to determine which patients are safe for discharge. PCT may have a role, as Dr. Breed mentioned, as one part of the decision making process, in concert with the heme-onc team. Be very cautious with these patients and with the MASCC and CISNE scores. ~Clay Smith
Source
Prognostic Value of Serum Procalcitonin Levels in Patients With Febrile Neutropenia Presenting to the Emergency Department. J Emerg Med. 2021 May;60(5):641-647. doi: 10.1016/j.jemermed.2020.12.010. Epub 2021 Jan 28.
