Author: Ellie Salinski, MD (Attending Emergency Physician, Crozer Chester Medical Center, Upland, PA) // Editor: Alex Koyfman, MD, & Justin Bright, MD
Anatomy & Definition
The left bundle branch arises from the Bundle of His, and subsequently is divided into the anterior and posterior fascicles. The anterior fascicle is usually supplied by septal perforators from the Left Anterior Descending artery, and the posterior fascicle typically has a dual supply from septal perforators from the Left Anterior Descending artery and the Posterior Descending artery (arising from the Right Coronary).
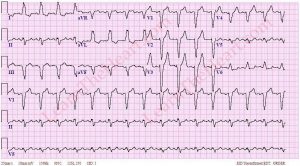
Electrocardiographically, a LBBB is defined as QRS duration greater than or equal to 120 ms; a broad-notched or slurred R wave in leads I, aVL, V5, and V6; absent Q waves in leads I, V5, and V6; and an R peak time >60 ms in leads V5 and V6 but normal in leads V1 to V3 (1). LBBB can be transient and/or rate-related (1). These morphologic changes make it difficult to discern whether or not a patient presenting to the emergency department with chest pain is experiencing a STEMI.
In the setting of AMI, a new LBBB is rare and would only be the result of either a localized lesion just distal the Bundle of His or an extensive infarction involving both fascicles (2). A LBBB in the setting of AMI is more often an indicator of underlying structural heart disease, and may result from an “aging or fibrotic conduction system, chronic ischemic heart disease, left ventricular hypertrophy, remodeling resulting from congestive heart failure, or valvular disease” (2).
Epidemiology
Few patients presenting to the ED with suspected AMI have a LBBB, ranging from only 1-9% reported in prior studies (2-6). Patients with LBBB are more likely to be older, to be female, and to have a history of pre-existing cardiovascular disease, hypertension, and congestive heart failure. Notably, some studies with older data have shown that patients with LBBB have a higher long-term mortality than those without a LBBB (3, 4). Other more recent studies have failed to show increased mortality with a LBBB alone, and have suggested that it may be a marker of overall cardiac risk, rather than a cause (5, 6).
Sgarbossa Criteria
Due to frequent presence of ST-elevation in anteroseptal or inferior leads, the presence of a LBBB is commonly thought to impede the clinician’s ability to detect a STEMI on EKG. In 1996, Dr Sgarbossa reported 3 criteria that could help identify which patients with LBBB may be having an AMI (7):
1) ST-segment elevation ≥1 mm concordant with the QRS complex in any lead (5 points)
2) ST-segment depression ≥1 mm in lead V1, V2, or V3 (3 points)
3) ST-segment elevation ≥5 mm discordant with the QRS complex in any lead (2 points)
A total score ≥3 was found to be highly specific (98%) for the diagnosis of AMI; its sensitivity, however, was only 20% (8). Subsequent validation studies showed that patients meeting Sgarbossa concordance criteria were more likely to be having an AMI, and had similar or higher mortality rates compared with STEMI patients, vs lower mortality than STEMI patients in those who did not have concordance (9, 10, 11). The take-home message is that Sgarbossa criteria are very specific but not sensitive (8). Notably, they have “similar usefulness whether the LBBB is new or old” (2).
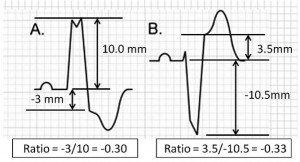
Smith, et al reported a new rule to replace the 3rd Sgarbossa criterion with the ST-segment elevation to S-wave depth (ST/S ratio): excessive relative discordance exists if the ST/S ratio is less than -0.25. This modified Sgarbossa rule increased sensitivity of the test to 91%, although specificity dropped to 90% when using the “weighted rule” (Sgarbossa >3) (12). It has yet to be validated, and has not been widely adopted into general practice.
The Evolution of STEMI Guidelines
The 1996 and 2004 AHA STEMI guidelines listed a new or presumed LBBB to be a STEMI equivalent. These prior guidelines were based on older data in the fibrinolytic era, used cardiac enzymes to define the presence of AMI, and many did not utilize Sgarbossa criteria (13). Cardiac biomarkers may be elevated in nonischemic cardiac disorders, as well as a variety of noncardiac conditions such as renal failure, sepsis, and pulmonary embolism (13). As such, using positive cardiac biomarkers alone to diagnose AMI in patients with LBBB may “overestimate the prevalence of the disease” (13). Chang et al, who did not employ Sgarbossa criteria, reported no difference in rates of AMI in patients with and without LBBB (regardless of chronicity) (14). Kontos, et al, however, found that concordant ST changes in the setting of LBBB were the most important predictor of AMI and 30-day mortality, whereas new or presumably new LBBB were neither (11).
In the era of PCI, there have been several studies that suggest that LBBB alone is not predictive of those patients who will have angiographic evidence of AMI. In a prospective registry study, Larson et al reported the rates of false activation of cardiac cath lab in 1,335 patients with suspected STEMI (15). In total, only 14% did not have a culprit lesion by angiography. In the 36 patients (2.6% of total patients) who had a new or presumed new LBBB, 44% of those patients did not have a culprit lesion, and 36% had negative cardiac biomarkers. In a retrospective registry study, Jain et al evaluated patients presenting with STEMI who had a new or presumed new LBBB (16). Out of 832 patients with STEMI, 36 (4%) had a new or presumed new LBBB. Only 14 of those patients had Acute Coronary Syndrome, and 5 of those had culprit lesions (2 went to CABG).
The presence of a LBBB in conjunction with concordance by Sgarbossa criteria, however, has been shown to be predictive of those patients who will have culprit coronary lesions. Lopes et al reported that 71.4% of patients with a new LBBB and concordant ST elevation had an occluded coronary artery, whereas only 44.1% of patients with a new LBB without concordant ST elevation had an occluded coronary artery (17). In the 5 patients who had a culprit lesion in the study by Jain et al., a Sgarbossa score of greater than or equal to 5 had 100% specificity (although 14% sensitivity) (16).
There have been several review articles that have detailed this more recent evidence, and implored the AHA to reconsider using LBBB alone as a criterion for emergent PCI (2, 18). In 2013, AHA updated these guidelines, and removed LBBB as a criterion for emergent PCI. “New or presumably new LBBB at presentation occurs infrequently, may interfere with ST-elevation analysis, and should not be considered diagnostic of acute myocardial infarction (MI) in isolation” (19). These guidelines made only a passing reference to Sgarbossa criteria.
A Proposed Algorithm (Am Heart J 2013)
A group of authors – including Dr Sgarbossa – caution that the new STEMI guidelines “fail to recognize that some patients with LBBB do have STEMI, and delaying reperfusion therapy in this population could be fatal” (13). They propose an algorithm that implements Sgarbossa criteria (and the modified criteria), takes into account hemodynamic instability, and utilizes serial electrocardiograms, enzymes, and echocardiography to help risk stratify those patients with LBBB and symptoms of ACS (13).
Summary
LBBB, although traditionally thought to be a STEMI equivalent, has recently been removed from AHA STEMI guidelines as an indication for catheterization lab activation. LBBB is associated with a variety of cardiac co-morbidities, and may or may not be an independent risk factor for AMI. Sgarbossa criteria are very specific for detecting AMI in patients with LBBB regardless of chronicity, and have been associated with higher mortality. In patients with a LBBB and suspected AMI, the presence of hemodynamic instability and/or the presence of concordance by Sgarbossa criteria should prompt strong consideration for emergent PCI.
References
1. Kumar V, Venkataraman R, Aljaroudi W, et al. Implications of left bundle branch block in patient treatment. Am J Cardiol 2013;111(2):291-300.
2. Neeland IJ, Kontos MC, et al. Evolving Considerations in the Management of Patients With Left Bundle Branch Block and Suspected Myocardial Infarction. J Am Coll Cardiol 2012; 60:96–105.
3. Bansilal S, Aneja A, Mathew V, et al. Long-term cardiovascular outcomes in patients with angina pectoris presenting with bundle branch block. Am J Cardiol 2011;107:1565–70.
4. Bauer GE, Julian DG, Valentine PA. Bundle-branch block in acute myocardial infarction. Br Heart J 1965;27:724 –30.
5. Stenestrand U, Tabrizi F, Lindback J, Englund A, Rosenqvist M, Wallentin L. Comorbidity and myocardial dysfunction are the main explanations for the higher 1-year mortality in acute myocardial infarction with left bundle-branch block. Circulation 2004;110:1896–902.
6. Yeo KK, Li S, Amsterdam EA, et al. Comparison of clinical characteristics, treatments and outcomes of patients with ST-elevation acute myocardial infarction with versus without new or presumed new left bundle branch block (from NCDR). Am J Cardiol 2012;109:497–501.
7. Sgarbossa EB, Pinski SL, Barbagelata A, et al. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. GUSTO-1 (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) Investigators. N Engl J Med 1996;334(8):481-7.
8. Tabas JA, Rodriguez RM, Seligman HK, et al. Electrocardiographic criteria for detecting acute myocardial infarction in patients with left bundle branch block: a meta-analysis. Ann Emerg Med 2008;52(4): 329-36.
9. Wong CK, French JK, Aylward PE, et al. Patients with prolonged ischemic chest pain and presumed-new left bundle branch block have heterogeneous outcomes depending on the presence of ST-segment changes. J Am Coll Cardiol 2005;46(1):29-38
10. Al-Faleh H, Fu Y, Wagner G, et al. Unraveling the spectrum of left bundle branch block in acute myocardial infarction: insights from the Assessment of the Safety and Efficacy of a New Thrombolytic (ASSENT 2 and 3) trials. Am Heart J 2006;151(1):10-5.
11. Kontos MC, Hammad AA, Chau VQ, et al. Outcomes in patients with chronicity of left bundle branch block with possible acute myocardial infarction. Am Heart J 2011;161:698-704.
12. Smith SW, Dodd KW, Henry TD, et al. Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ratio in a modified Sgarbossa rule. Ann Emerg Med 2012;60(6):766-76.
13. Cai Q, Mehta N, Sgarbossa EB, et al. The left bundle-branch block puzzle in the 2013 ST-elevation myocardial infarction guideline: From falsely declaring emergency to denying reperfusion in a high-risk population. Are the Sgarbossa Criteria ready for prime time? Am Heart J 2013;166:409-13.
14. Chang AM, Shofer FS, Tabas JA, et al. Lack of association between left bundle-branch block and acute myocardial infarction in symptomatic ED patients. Am J Emerg Med 2009;27(8):916-21.
15. Larson DM, Menssen KM, Sharkey SW, et al. “False-positive” cardiac catheterization laboratory activation among patients with suspected ST-segment elevation myocardial infarction. JAMA 2007;298(23): 2754-60.
16. Jain S, Ting HT, Bell M, et al. Utility of left bundle branch block as a diagnostic criterion for acute myocardial infarction. Am J Cardiol 2011;107(8):1111-6.
17. Lopes RD, Siha H, Fu Y, et al. Diagnosing acute myocardial infarction in patients with left bundle branch block. AmJCardiol 2011;108(6):782-8.
18. Rokos, IC, French WJ, Mattu A, et al. Appropriate cardiac cath lab activation: Optimizing electrocardiogram interpretation and clinical decision making for acute ST-elevation myocardial infarction. Am Heart J 2010; 160:995-1003.
19. O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013;127(4):e362-425.








7 thoughts on “Left Bundle Branch Block in Myocardial Infarction: An Update”
None of the research quoted here except the modified Sgarbossa paper uses angiographic occlusion as its outcome measure. Thus, they underestimate the sensitivity of the ECG. For instance, in the study by Jain mentioned above, of 892 patients referred for angiography, 36 had new LBBB and myocardial infarcton, but only 5 had true STEMI (coronary occlusion). Only this study by Smith et al. (http://download.journals.elsevierhealth.com/pdfs/journals/0196-0644/PIIS0196064412013686.pdf) studied patients with occlusion and compared them to those without.
Read the entire discussion that Smith modified paper.
Pingback: The LITFL Review 154 - LITFL