Authors: Dayna Staiert, MD and Braden McIntosh, MD (Louisiana State University Health Sciences Center-New Orleans School of Medicine, Emergency Medicine Residency Program, Baton Rouge Campus, Baton Rouge, Louisiana) // Edited by: Alex Koyfman, MD (@EMHighAK) and Brit Long, MD (@long_brit)
Case
A 35-year-old female with no significant past medical history presents to the Emergency Department for syncope. She was at work when she felt lightheaded and passed out. She slumped over in her chair but did not fall or hit her head. Per her co-workers, she was unconscious for less than one minute and rapidly returned to baseline. She denies any chest pain, shortness of breath, abdominal pain, menorrhagia, or previous history of syncope.
Initial vitals include T 36.8 C, HR 72, BP 108/70, Sat 99% on RA, RR 14.
When you arrive in the room, she is sitting in bed and is well appearing. Her neurological exam is normal, and her cardiac exam is unremarkable with no murmurs. Her skin is warm and well perfused and has no conjunctival pallor. Her ECG shows normal sinus rhythm. A CBC, BMP, troponin, and urine pregnancy were ordered in triage and are pending. Patient says she feels much better and is requesting to go home.
Background
Syncope is a transient loss of consciousness with spontaneous return to baseline neurologic function requiring no resuscitative efforts. Syncope accounts for 1-3% of all emergency department visits and 6% of all hospitalizations.1-4 Nearly ¼ of the population experience syncope during their lifetime.5 Approximately ⅓ of all syncope visits result in hospitalization.6 There are many common causes of syncope including vasovagal, cardiac, orthostatic, neurologic, and medication-related events. Cardiac causes of syncope include arrhythmias such as AV block, SVT, abnormal atrial rhythms and cardiac pause and structural heart disease such as valvular disorders, hypertrophic obstructive cardiomyopathy, and channelopathies. The cause of syncope is unknown in up to 50% of patients, and vasovagal syncope accounts for 25% of cases.1 Certain syncope causes are more dangerous than others and are associated with increased risk of death and adverse events. Cardiac cause of syncope increases risk of death by 10% within 6 months following the event.7 Neurologic cause of syncope such as TIA or CVA increases rate of death by 50% when compared with patients who never experienced syncope.7 Syncope is a common ED complaint with many serious causes. Therefore, the goal as an EM provider is to determine which patients are low risk syncope and are safe for discharge home.
Pearls
There are factors that may help ED physicians determine category of risk:
Many factors can place a patient in a lower risk category for syncope such as age less than 40 years old, previous history of syncope with similar episodes to the current episode, and syncope while standing or with prodromal symptoms making vasovagal or stimulus syncope more likely.8 Conversely, other factors place patients in a higher risk category such as syncope during exertion, preceding symptoms such as chest pain, family history of sudden death, and heart failure or history of arrythmia.8
Risk Assessment Tools are available:
Multiple Risk assessment tools exist to risk stratify patients with syncope. The San Francisco Syncope Rule (SFSR) is one such tool that can provide a structured thought process regarding which patients are higher risk and would benefit from admission. A study compared physician judgement to the SFSR and found that although physician judgement is good at determining high risk patients who present with syncope, the physicians still admit a large number of low risk patients.5
San Francisco Syncope Rule:
- CHF history
- Hct < 30%
- ECG or cardiac monitoring abnormal
- SOB history
- SBP < 90 mm Hg at triage
From Dr. Hanson at Hanson’s Anatomy:
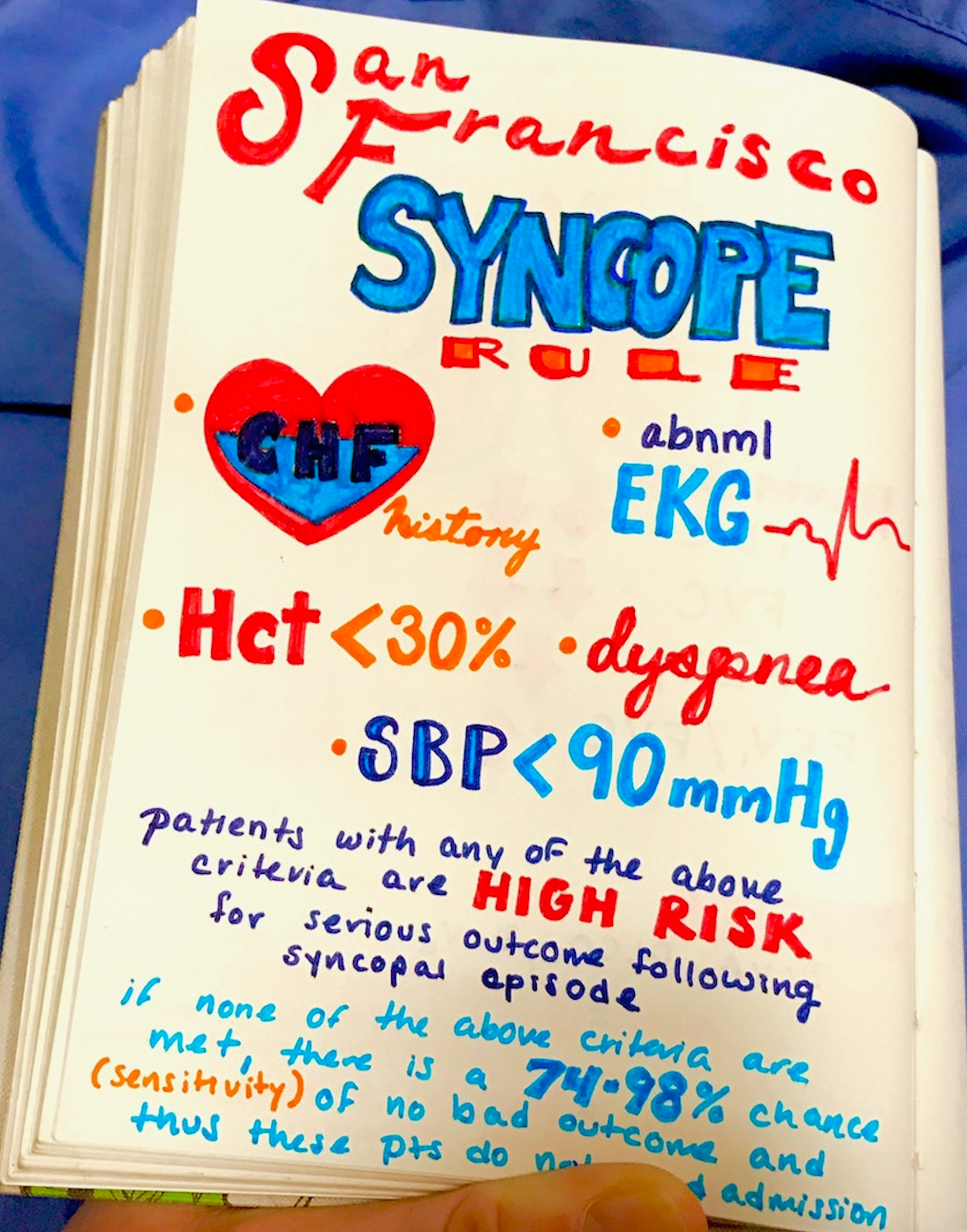
Patients with any of the following predictors are considered high risk for serious outcomes at 7 and 30 days.
The SRSR has not been externally validated and may fall short in elderly populations.5,6,9,10,14 Multiple studies have showed lower sensitivities and specificities within the 7-day window for serious outcomes than were initially reported. This may be especially important in elderly populations. One study showed multiple serious outcomes, most commonly arrhythmias, in elderly populations that were negative on the San Francisco Syncope Rule.14
The Intermediate-Risk Syncope (IRiS) Study11 examined patients in an intermediate risk group to determine adverse events. Intermediate risk group includes any one of the following:
- Any age
- Heart disease currently in stable condition (heart failure, previous MI)
- Comorbidities related to syncope that are in a stable condition
- No family history of SCD
- Symptoms not suggestive of neurally mediated syncope
- No chest pain or systolic murmur
- ECG abnormalities that were not high risk (abnormal QT interval, Brugada pattern, block with prolonged QRS or sinus bradycardia)
Patients that fell in this group had a 0.8% rate of serious outcomes. These patient’s may benefit from discharge or from observation instead of inpatient admission.11
ED Physicians Should Limit Lab Testing:
According to ACEP and the American College of Cardiology recommendations the only test recommended in all patients is a resting EKG.12,13 They do not recommend routine or comprehensive laboratory testing.12,13 A hemoglobin and hematocrit may be obtained to risk stratify a patient using San Francisco Syncope Rule. Additional testing is only recommended based on history findings.12 A study showed that patients diagnosed with vasovagal syncope had few serious outcomes and no deaths within 30 days following ED evaluation.1 Despite such data, many studies show that these patients received extensive workup, including 78% of patients receiving blood tests.1
Pitfalls
Syncopal Episodes Result in Excessive admissions:
30-50% of hospital admissions for syncope are discharged without a specific diagnosis other than syncope and collapse.9,15 Hospitalization for syncope costs $2 to $6 billion annually and can average upwards of $5300 per hospital stay.6,16 Admission for syncope does not increase one-year survival.9 In one study, acute intervention for a patient admitted for syncope happened in only 1% of patients.17 Early outpatient evaluation would be a safe option for most patients who are low risk and in whom ED evaluation does not reveal a specific diagnosis.17
Over-imaging is Common:
Neuroimaging is not routinely recommended in syncope. Current data shows that there has been an increase in utilization of CT or MRI to nearly 50% of syncope cases seen in the ED.3 The current recommendations by the ACA/AHA regarding head CT and MRI is that there is no benefit and it’s not routinely recommended in the absence of focal neurological deficit.12T he ACEP clinical policy does not recommend routine screening with advanced imaging such as CT or MRI.13 Imaging is indicated when there is a concern for injury due to syncope. However, in patients with a normal neurological exam, further imaging such as Head CT or MRI is not indicated. A recent study showed that less than 4% of patients who received a CT or MRI in their syncope evaluation had an abnormal finding. Patients more likely to have an abnormal finding had a focal neuro deficit, history of malignancy, hypertension, or age greater than 60.18
Routine Screening for Pulmonary Embolism is not Necessary:
The PESI trial showed that pulmonary embolism was present in hospitalized patients who presented for first time syncope in up to 17% of patients.19 However, repeat studies found a much lower prevalence of PE in hospitalized patients.20 The original study only examined hospitalized patients.19 Further studies have shown PE was present in less than 1% of all patients presenting with syncope and less than 3% of hospitalized patients.20 These articles suggest that excluding PE in all patients with syncope may lead to false positive tests in D-dimers and CTA’s with potential to cause harm to patients.20Although pulmonary embolism should be considered in syncope patients, it does not need to be routinely ruled out unless history or physical exam is concerning for PE.
Orthostatic Vital Signs are not Diagnostic of Syncope:
Orthostatic vital signs are often obtained to determine a cause of syncope. According to the AHA/ACA, orthostatic vital signs should be obtained on patients presenting with syncope.12 Positive orthostatic vital signs include a decrease in blood pressure by 20 mm Hg or a reflex tachycardia of 20 bpm as a patient transitions from supine to standing position. Orthostatic vital signs are to be measured after a person has been standing for 3 minutes. Patients may be considered “orthostatic” due to experiencing symptoms despite having normal vital signs. The studies show that having “positive” orthostatic vital signs is not an independent predictor of mortality or serious events.21 Orthostatic vital signs are not specific as a cause of syncope. Studies show that elderly patients may be asymptomatic despite having positive orthostatic vital signs.13,21 Although commonly obtained orthostatic vital signs are not always diagnostic of syncope and may lead to missing a more serious cause of syncope. Therefore, orthostatic hypotension should be a diagnosis of exclusion in low risk patients.13
It is not Necessary to Order a Troponin for all Syncope Patients:
Troponin is often ordered as a standard lab in a syncope workup, especially in elderly patients. However, studies show that an elevated troponin is not predictive of cardiac syncope, nor does elevated troponin predict the prognosis of a patient with cardiac syncope.22 Despite this data, patients who had non-cardiac syncope with elevated troponin did have a poorer prognosis.22 Dysrhythmia is a common cause of cardiac syncope but does not often cause elevated troponin levels.19,22 Although, the Canadian Syncope Arrhythmia Risk Score includes elevated troponin levels in its calculation, most of its factors are based on history and ECG.4 If concerned for ACS based on patients history or if the patient has evidence of ischemia on ECG a troponin can be obtained as part of syncope evaluation.
Case Conclusion
The patient reported feeling well. Her EKG was normal. Lab work was unremarkable, and urine pregnancy test was negative. She did not have any concerning history findings such as syncope during exertion or previous episodes of syncope. She did not have any past medical history such as CHF or history of arrhythmia. Per SFSR, the patient was determined to be low risk. Per Canadian Syncope Arrhythmia Score, she was considered very low risk for arrhythmia. Patient was discharged with a diagnosis of vasovagal syncope and advised to follow up with her PCP within 3 days.
Key Points:
- Cause of syncope can often be determined by history and physical alone. Only an ECG is recommended testing in all patients.
- Multiple Risk Assessment tools exist which can guide disposition.
- Admission can often be avoided if patients can have close follow up with their PCP. Hospital admission often does not lead to a more specific diagnosis.
- A troponin should not be obtained routinely in all patients with syncope unless concern for ischemia/ACS is present.
- Positive orthostatic vital signs may cause early closure and are non-specific.
- CT and MRI should be reserved for patients with other risk factors and focal neurologic deficits and shouldn’t be routinely ordered in syncope.
- Pulmonary embolism as a cause of syncope is not as common as previously thought, occurring in less than 1% of patients with syncope.
- Physician judgment is good for identifying patients with low risk syncope. We should apply that same judgment to determining which patients are safe to discharge and which can skip the extensive workup including labs and imaging.
References/Further Reading:
- Toarta C, Mukarram M, Diercks D, et al. Syncope Prognosis Based on Emergency Department Diagnosis: A Prospective Cohort Study. Academic Emergency Medicine (AEM)[serial online]. April 1, 2018;25(4):388-396. Available from: E-Journals, Ipswich, MA. Accessed May 1, 2018.
- Tintinalli, Judith E. Emergency Medicine: a Comprehensive Study Guide. McGraw-Hill, 2011.
- Probst M, Kanzaria H, Gbedemah M, Richardson L, Sun B. National trends in resource utilization associated with ED visits for syncope. The American Journal Of Emergency Medicine [serial online].August 1, 2015;33(8):998-1001. Available from: E-Journals, Ipswich, MA. Accessed May 1, 2018.
- Thiruganasambandamoorthy V, Stiell I, Baumann B, et al. Predicting Short‐term Risk of Arrhythmia among Patients With Syncope: The Canadian Syncope Arrhythmia Risk Score. Academic Emergency Medicine (AEM)[serial online]. November 1, 2017;24(11):1315-1326. Available from: E-Journals, Ipswich, MA. Accessed May 1, 2018.
- Quinn J, Stiell I, McDermott D, Kohn M, Wells G. The San Francisco Syncope Rule vs physician judgment and decision making. The American Journal Of Emergency Medicine[serial online]. October 1, 2005;23(6):782-786. Available from: E-Journals, Ipswich, MA. Accessed May 1, 2018.
- Snead G, Wilbur L. Can the San Francisco Syncope Rule predict short-term serious outcomes in patients presenting with syncope? Annals of Emergency Medicine[serial online]. September 2013;62(3):267-268. Available from: MEDLINE, Ipswich, MA. Accessed May 1, 2018
- Quinn J, McDermott D, Stiell I, Kohn M, Wells G. Prospective Validation of the San Francisco Syncope Rule to Predict Patients With Serious Outcomes. Annals of Emergency Medicine [serial online]. May 1, 2006;47(5):448-454. Available from: E-Journals, Ipswich, MA. Accessed May 1, 2018.
- Costantino G, Sun B, Furlan R, et al. Syncope clinical management in the emergency department: a consensus from the first international workshop on syncope risk stratification in the emergency department. European Heart Journal[serial online]. n.d.;37(19):1493-1498. Available from: Biological Abstracts, Ipswich, MA. Accessed May 11, 2018.
- Nishijima D, Lin A, Sun B, et al. ECG Predictors of Cardiac Arrhythmias in Older Adults With Syncope. Annals of Emergency Medicine [serial online]. April 1, 2018;71(4):452-461.e3. Available from: E-Journals, Ipswich, MA. Accessed May 1, 2018.
- Serrano L, Hess E, Decker W, et al. Accuracy and Quality of Clinical Decision Rules for Syncope in the Emergency Department: A Systematic Review and Meta-analysis. Annals of Emergency Medicine [serial online].October 1, 2010;56(4):362-373.e1. Available from: E-Journals, Ipswich, MA. Accessed May 1, 2018.
- Numeroso F, Mossini G, Giovanelli M, Lippi G, Cervellin G. Short-term Prognosis and Current Management of Syncopal Patients at Intermediate Risk: Results from the IRiS (Intermediate-Risk Syncope) Study. Academic Emergency Medicine [serial online]. August 2016;23(8):941-948. Available from: CINAHL Complete, Ipswich, MA. Accessed July 4, 2018.
- Shen W, Sheldon R, Yancy C, et al. 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients With Syncope: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Journal of The American College Of Cardiology[serial online]. August 1, 2017;70(5):e39-e110. Available from: MEDLINE, Ipswich, MA. Accessed May 1, 2018.
- Huff J, Decker W, Jagoda A, et al. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with syncope. Journal of Emergency Nursing: JEN: Official Publication of the Emergency Department Nurses Association[serial online]. December 2007;33(6):e1-e17. Available from: MEDLINE, Ipswich, MA. Accessed July 4, 2018
- Schladenhaufen R, Feilinger S, Pollack M, Benenson R, Kusmiesz A. Application of San Francisco Syncope Rule in elderly ED patients. The American Journal of Emergency Medicine [serial online]. September 1, 2008;26(7):773-778. Available from: E-Journals, Ipswich, MA. Accessed May 1, 2018.
- Probst M, Hess E, MarkCourtney D, et al. Development of a Patient Decision Aid for Syncope in the Emergency Department: the SynDATool. Academic Emergency Medicine (AEM)[serial online]. April 1, 2018;25(4):425-433. Available from: E-Journals, Ipswich, MA. Accessed May
- Lin M, Wolfe R, Shapiro N, Novack V, Lior Y, Grossman S. Observation vs admission in syncope: can we predict short length of stays? The American Journal of Emergency Medicine[serial online]. November 1, 2015;33(11):1684-1686. Available from: E-Journals, Ipswich, MA. Accessed May 1, 2018.
- Manheimer E, Pacio G, Ferrick K. Limited yield of hospitalization for the evaluation of syncope in patients presenting to an urban tertiary medical center. The American Journal of Emergency Medicine[serial online]. September 1, 2014;32(9):1113-1116. Available from: E-Journals, Ipswich, MA. Accessed May 1, 2018.
- Ozturk K, Soylu E, Bilgin C, Hakyemez B, Parlak M. Predictor variables of abnormal imaging findings of syncope in the emergency department. International Journal of Emergency Medicine. 2018;11:16. doi:10.1186/s12245-018-0180-0.
- Touray S. Prevalence of pulmonary embolism in patients with syncope: findings from the Pulmonary Embolism in Syncope Italian Trial (PESIT).Breathe[serial online]. March 2017;13(1):53. Available from: CINAHL Complete, Ipswich, MA. Accessed May 2, 2018.
- Costantino G, Ruwald M, Casazza G, et al. Prevalence of Pulmonary Embolism in Patients With Syncope. JAMA Internal Medicine[serial online]. n.d.;178(3):356-362. Available from: Biological Abstracts, Ipswich, MA. Accessed May 1, 2018.
- Bloom A, Devlin J. Discriminatory Value of Orthostatic Vital Signs in the Emergency Department Evaluation of Syncope. Annals of Emergency Medicine[serial online]. September 1, 2017;70(3):438-439. Available from: E-Journals, Ipswich, MA. Accessed May 1, 2018
- Thiruganasambandamoorthy V, Perry J. High-sensitivity cardiac troponin T in isolation has limited diagnostic utility in identifying cardiac causes of syncope. Evidence Based Medicine[serial online]. August 2015;20(4):146. Available from: CINAHL Complete, Ipswich, MA. Accessed May 1, 2018.









2 thoughts on “Low Risk Syncope – Pearls and Pitfalls”
Pingback: Länkar v38-39 | Internmedicin
Pingback: Orthostatics – Helpful or Useless? – JournalFeed