Written by: David Cisewski, MD (@DHCisewski – EM Resident Physician, Icahn School of Medicine at Mount Sinai) // Edited by: Manpreet Singh, MD (@MPrizzleER), Alex Koyfman, MD (@EMHighAK), and Brit Long, MD (@long_brit)
emDocs is proud to present a new series by Dr. David Cisewski evaluating pain management in the emergency department. One of our most important roles in the ED is not only resuscitation and risk stratification, but treating pain. This series is here to help! Each post will be accompanied by an infographic for further use.
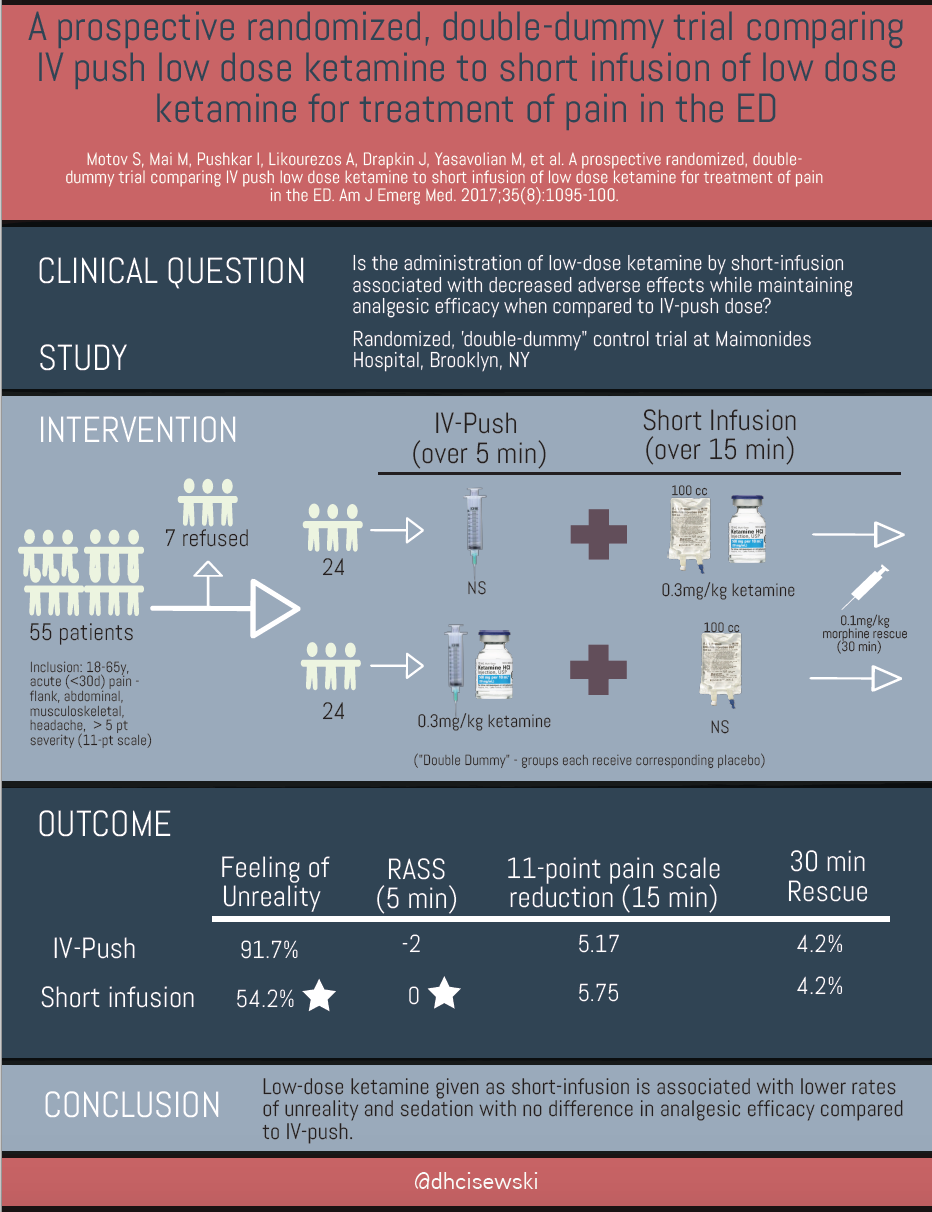
A prospective randomized, double-dummy trial comparing IV push low dose ketamine to short infusion of low dose ketamine for treatment of pain in the ED
Motov S, Mai M, Pushkar I, Likourezos A, Drapkin J, Yasavolian M, et al. A prospective randomized, double-dummy trial comparing IV push low dose ketamine to short infusion of low dose ketamine for treatment of pain in the ED. Am J Emerg Med. 2017;35(8):1095-100. PMID: 28283340
One-Liner
Low-dose ketamine given as short-infusion is associated with lower rates of unreality and sedation with no difference in analgesic efficacy compared to IV-push.
Study Characteristics
- Clinical question – Is the administration of low-dose ketamine (LDK) by slow infusion (SI) associated with decreased rates of adverse effects while maintaining analgesic efficacy when compared to intravenous push (IVP) dose?
- Design – Prospective, randomized, double-blind, double- dummy trial
- Setting – Emergency room, Maimonides Hospital, Brooklyn, NY
- Patient/Population: 55 patients between 18 to 65 years old who presented to the ED primarily for management of acute (<30d) pain – flank, abdominal, musculoskeletal, or headache – with an intensity of 5 or greater on a standard 0 to 10 numeric rating scale . Patients excluded included pregnancy, breast-feeding, altered mental status, allergy to ketamine, weight <46 kg or >115 kg, unstable vital signs (systolic blood pressure <90 or >180 mm Hg, pulse rate <50 or >150 beats/min, and respiration rate <10 or >30 breaths/min), medical history of acute head or eye injury, seizure, intracranial hypertension, renal or hepatic insufficiency, alcohol or drug abuse, psychiatric illness, recent (4 h before) analgesic use.
- Intervention: Participants received intravenous LDK of 0.3 mg/kg by one of two randomized options: IVP given over 5 min or mixed in 100 ml normal saline solution and given via SI over 15 min. Each participant also received a corresponding placebo consistent with the opposing arm of the randomization (double-dummy). The two mixtures administered routes were started simultaneously. Rescue morphine (0.1 mg/kg IV) was given 30 min to anyone requiring further analgesia. Feelings of dissociation (Side Effects Rating Scale for Dissociative Anesthetics (SERSDA)) and overall sensation of sedation (Richmond Agitation-Sedation Scale (RASS)) were measured as primary outcomes. Reduction in pain scale was measured on an 11-point numerical rating scale (NRS) and requirement for rescue analgesic was measured as a secondary outcome.
- Outcomes: The overall feeling of unreality was significantly higher in the IVP group: 91.7% vs 54.2% (% difference – 37.5%; p = 0. 008) with the difference was most marked at 5 and 15 min. IVP also resulted in an increased level of sedation during the procedure. Both the IVP and SI resulted in equivalent levels of pain reduction and requirement for rescue analgesia.
Quality Assessment
This was a well-conducted randomized control trial conducted by a team well versed in the use of SDK. The utilization of the double-dummy technique offered further elimination of any potential confounding factors associated with the delivery of each arm of the trial individually.
The Upshot
In 1971, twenty-four years before the release of oxycontin, Dr. Max Sadove released his landmark study regarding the safety and efficacy of using SDK (0.44 mg/kg) to treat acute postoperative pain. For over 45 years have debated the use of SDK for acute treatment of pain within the emergency room. Fear of side effects, particularly the stigma associated with the feeling of unreality, have been the major hindrance. Though a relatively small study size in a single-center ED (80% power), this study by Motov, et al offers further knowledge on the safe, yet effective use of ketamine for analgesia when give over a 15 minute duration.
One major obstacle to the use of slow infusion LDK, as stated by the author, is the practicality of having infusion pumps set up by nursing staff in busy ED’s. Many have offered the suggestion that the LDK/100cc NS solution run as a drip would safely approximate the delivery over 15 minutes as well.
Further Reading
- emDOCs – Ketamine for Analgesia in the ED by Reuben Strayer
- ACEP – Policy Statement on SDK use in ED: Sub-dissociative dose ketamine for analgesia
- ACEP-prepared Policy Resource Education Paper (PREP) on SDK: “Sub-dissociative Dose Ketamine for Analgesia.”
- Emergency Physicians Monthly Interview with Nicholas Genes, MD PHD and Sergey Motov, MD: Motov’s Cocktails: Sub-Dissociative Ketamine
- Sadove MS, Shulman M, Hatano S, Fevold N. Analgesic effects of ketamine administered in subdissociative doses. Anesth Analg. 1971;50(3):452-7. PMID: 5103784
- Skeptics Guide to Emergency Medicine (SGEM):
- R.E.B.E.L EM – Low-Dose Ketamine for Acute Pain in the ED: IV Push vs Short Infusion?
- EM Cases Journal Jam – Low Dose Ketamine Analgesia
- Peds EM Morsels – Ketamine for Analgesia







1 thought on “Pain Profiles: Ketamine for Analgesia”
Pingback: emDOCs.net – Emergency Medicine EducationPain Profiles: The GERIKET Trial and Geriatric Analgesia - emDOCs.net - Emergency Medicine Education