Authors: Zachary Sletten, MD (EM Attending, Brooke Army Medical Center) and Simon Sarkisian, DO (EM Attending, Cooper University Hospital/US Army, Camden, NJ) // Reviewed by: Alexander Y. Sheng, MD, MHPE (@theshenger); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
You are a busy emergency medicine (EM) attending physician, and you hear about a facial laceration that just checked in. The intern asks you for help repairing the laceration, and you eagerly accompany them into the room excited to endow them with your wisdom on laceration repair. After stepping into the room, you realize you might be in over your head (no pun intended). This is not your run of the mill facial laceration.
The series will review the repair of head, eyes, ears, nose, and throat (HEENT) lacerations, with a focus on the areas where emergency physicians tend to struggle. Today we look at eyelid lacerations.
Case
A 12-year-old female is brought to your emergency department after being bitten by a dog with lacerations to her cheek and eyelid. As you examine the patient, you try to recall which lacerations will require repair by a surgeon and begin considering what your approach might be to repair.
Eyelid Lacerations

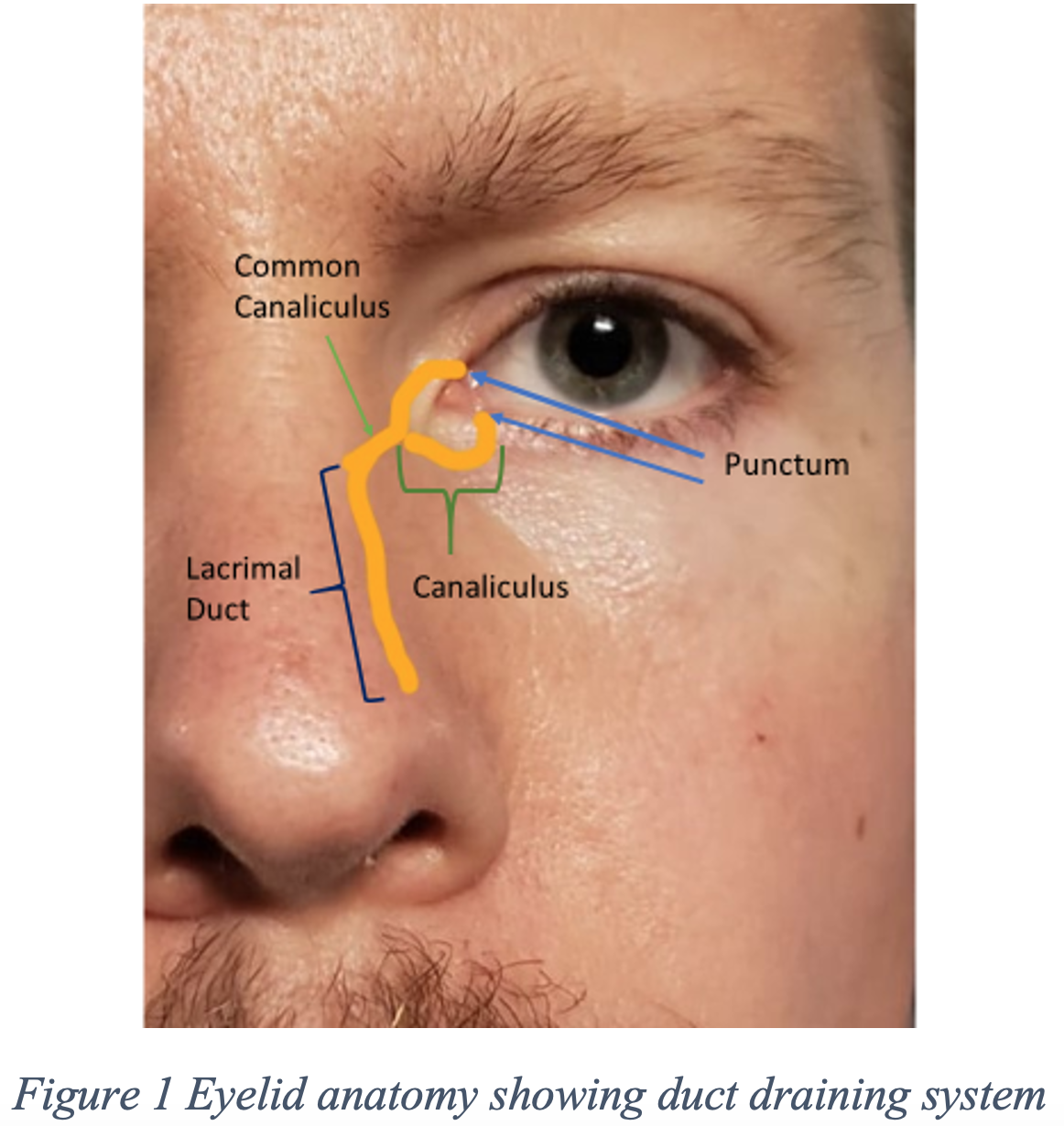
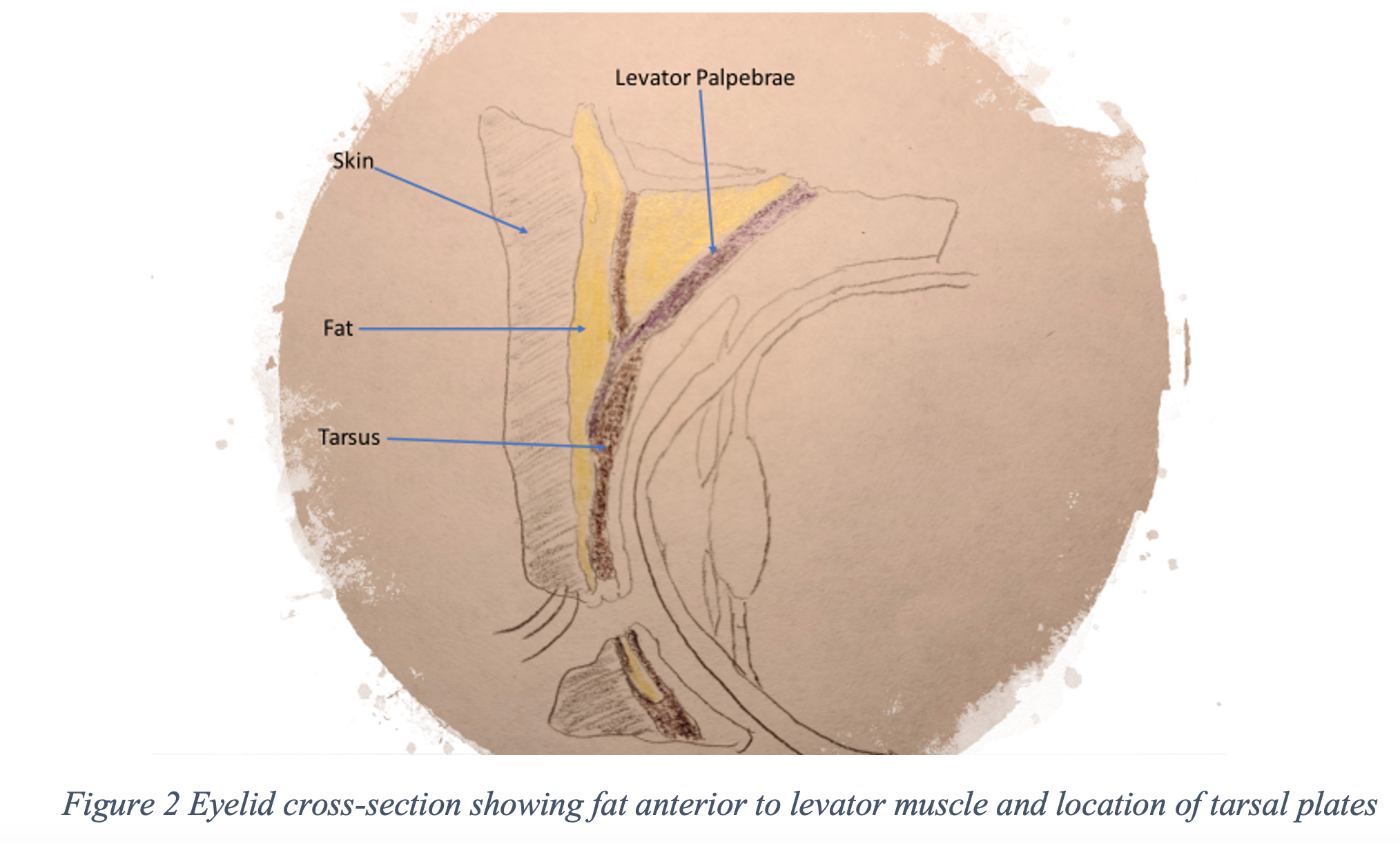
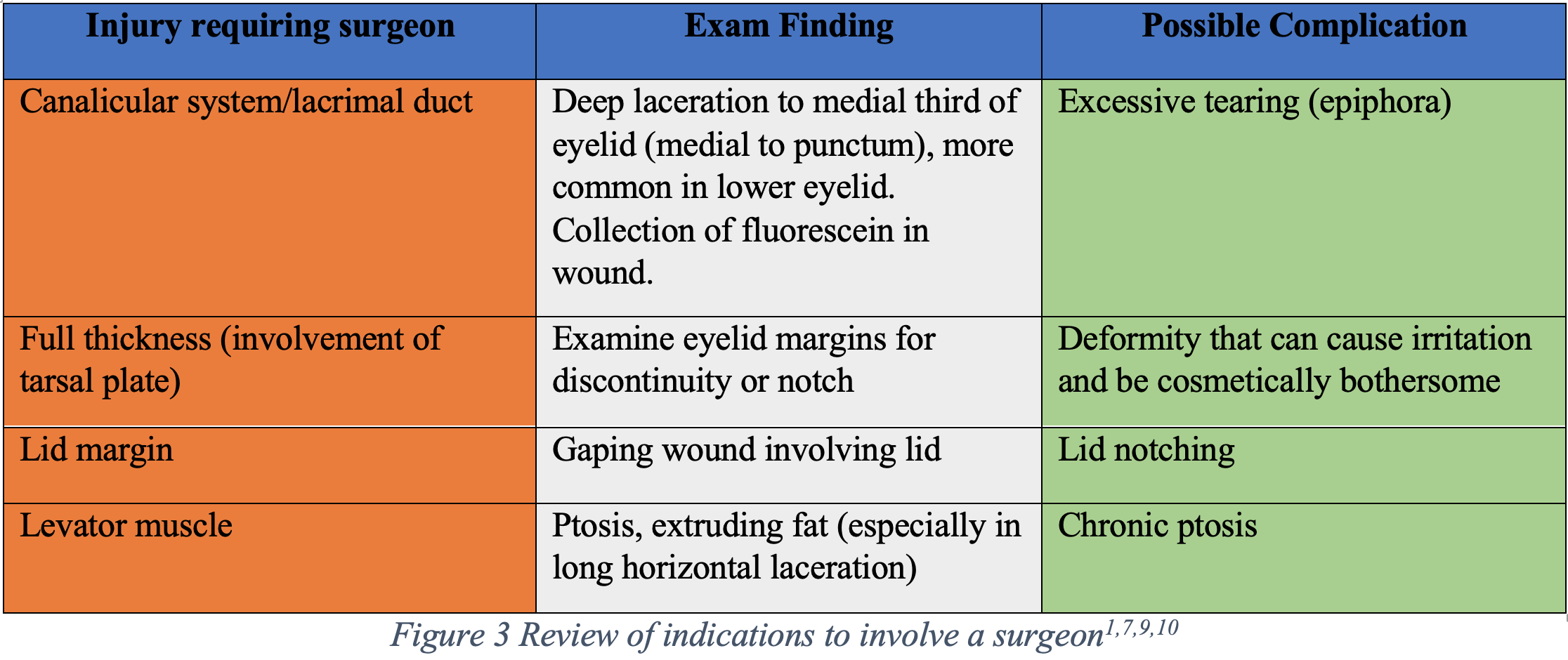
Proper management of eyelid lacerations requires careful examination and an understanding of pertinent anatomy (see figure 1 and 2 for reference). It is important to recognize lacerations which should be repaired by a specialist such as an ophthalmologist or oculoplastic surgeon to avoid poor outcomes and morbidity (reviewed in figure 3)1,7. Ensure the patient is not suffering from an open globe before a more detailed assessment of the eye so as not to apply pressure to the eye. Irrigate the eye and inspect for foreign bodies. Assess the depth and location of wounds. A surgeon should be consulted in cases with:
- Lacerations involving the eyelid margin
- Lacerations near the medial canthus concerning for canalicular system involvement
- Lacerations involving the lacrimal duct/sac
- Ptosis or protruding fat concerning for levator muscle involvement
- Full thickness lacerations/lacerations involving the tarsus
Repair of the wound should occur within 24-48 hours if possible. Although, there is recent literature to suggest repair can be delayed up to 6 days for certain injuries like lacerations involving the canalicular system1,8,9. For lacerations near the medial third of the eye where there is a suspicion for canalicular involvement, a fluorescein test can be performed which may demonstrate fluorescein collecting in the wound if the canicular system has been damaged. For full thickness lacerations (involving the tarsus) one should be diligent to evaluate for open globe injury.
Once more complicated injuries have been evaluated for and ruled out, repair of partial thickness lacerations can be performed in the emergency department. Given how thin the skin is, using 6-0 or 7-0 absorbable or non-absorbable sutures is recommended1,10. Pro tip: consider tying the tails of the sutures near the eye down with adjacent sutures to avoid irritation to the eye. This goes without saying but be careful not to puncture the eye with your needle. Although possible, the eyelid rarely gets infected due to its excellent blood supply11. Arrange for suture removal in 5-7 days.
That’s it for this week. Stay tuned for our next piece in the series.
References/Further Reading
1. Tintinalli JE, Ma OJ, Yealy DM, et al. Tintinalli’s emergency medicine: a comprehensive study guide. 2020.
2. Hollander JE, Richman PB, Werblud M, Miller T, Huggler J, Singer AJ. Irrigation in facial and scalp lacerations: does it alter outcome? Ann Emerg Med 1998;31:73-7.
3. Singer AJ, Gulla J, Hein M, Marchini S, Chale S, Arora BP. Single-layer versus double-layer closure of facial lacerations: a randomized controlled trial. Plast Reconstr Surg 2005;116:363-8; discussion 9-70.
4. Farion KJ, Russell KF, Osmond MH, et al. Tissue adhesives for traumatic lacerations in children and adults. Cochrane Database of Systematic Reviews 2002.
5. Holger JS, Wandersee SC, Hale DB. Cosmetic outcomes of facial lacerations repaired with tissue-adhesive, absorbable, and nonabsorbable sutures. Am J Emerg Med 2004;22:254-7.
6. Eyelid Injury. 30 OCT 2010. (Accessed 27 AUG 2020, at http://drbohra.blogspot.com/2010/10/eyelid-injury.html.)
7. Ko AC, Satterfield KR, Korn BS, Kikkawa DO. Eyelid and Periorbital Soft Tissue Trauma. Facial Plast Surg Clin North Am 2017;25:605-16.
8. Chu YC, Wu SY, Tsai YJ, Liao YL, Chu HY. Early Versus Late Canalicular Laceration Repair Outcomes. Am J Ophthalmol 2017;182:155-9.
9. Gordon AA, Tran LT, Phelps PO. Eyelid and orbital trauma for the primary care physician. Dis Mon 2020:101045.
10. Roberts JR, Custalow CB. Roberts and Hedges’ clinical procedures in emergency medicine and acute care. 2019.
11. Nelson CC. Management of eyelid trauma. Aust N Z J Ophthalmol 1991;19:357-63.







