Authors: Kayvan Moussavi, PharmD, BCCCP (Assistant Professor- Department of Pharmacy Practice, Marshall B. Ketchum University College of Pharmacy) and Scott Fitter, PharmD, BCCCP (Clinical Pharmacy Specialist- Emergency Department, Loma Linda University Medical Center) // Edited by: Tim Montrief, MD (@EMinMiami); Alex Koyfman, MD (@EMHighAK); and Brit Long, MD (@long_brit)
Case
A 70-year-old, 70 kg male presents to your ED with return of spontaneous circulation (ROSC) after a suspected STEMI. Patient received CPR for about 5 minutes, received one dose of epinephrine 1 mg via IO, and was intubated by paramedics. EKG was positive for inferior MI. Paramedics report that the last blood pressure they measured was 110/60 mmHg and heart rate was 60 bpm (sinus rhythm). As you are performing your initial patient assessment, the cardiologist arrives, examines the patient and EKG, then states she can take the patient to cath lab in about 5 minutes. Both of you note that the blood pressure is now 90/40 mmHg and heart rate is 49 bpm (sinus bradycardia). You check for a pulse and find one, but are worried that the patient may soon go into cardiac arrest. The cardiologist asks, “Can we start a vasopressor? Maybe norepinephrine?” You state that you will have to order norepinephrine from the pharmacy and that it will take 10-15 minutes to arrive. You start to wonder if there is something you can give now while waiting for the norepinephrine.
Introduction
Vasopressors are utilized to increase a patient’s blood pressure through effects on the heart or vascular smooth muscle, and are most often administered as continuous infusions [1]. Push-dose vasopressors, or push-dose pressors, refers to administration of intermittent, small doses of vasopressors to optimize a patient’s hemodynamic status [2, 3]. Commonly used push-dose vasopressors include epinephrine and phenylephrine [2, 3]. Push-dose administration is a long standing practice amongst anesthesiologists to resolve hypotension secondary to sedation or a surgical procedure [2]. Outside of the Operating Room (OR), push-dose pressors can be used in any clinical scenario in which hypotension could result in poor outcomes, such as: sepsis, trauma, emergent airway management, and cardiac arrest with ROSC [2-8]. Many of these patients will require further vasopressor administration, with push-dose vasopressors used as a bridge to continuous infusions.
Epinephrine is an alpha and beta-receptor agonist, which increases myocardial contraction, coronary vasodilation, and induces chronotropy [1-3]. These properties make epinephrine less ideal in patients who present with tachycardia or tachyarrhythmias. Push-dose epinephrine has onset of 1 minute and a duration of action of 5 to 10 minutes [2, 3]. Typical bolus doses of epinephrine range from 5 to 10 mCg repeated every 2 to 5 minutes to achieve hemodynamic goal (e.g. SBP>90 mmHg, MAP>65 mmHg, HR 60-90 bpm) [2, 3].
Phenylephrine is a pure alpha agonist that causes arterial vasoconstriction and an in increase systemic vascular resistance [1-3]. Phenylephrine has no direct chronotropic effects, which makes it an attractive option for patients that are hypotensive and tachycardic [1-3]. However, phenylephrine may induce baroreceptor-mediated, reflex bradycardia due to rapid increases in blood pressure [1]. Push-dose phenylephrine also has a rapid onset (1 minute) and slightly longer duration of action compared to epinephrine (10 to 20 minutes vs. 5 to 10 minutes) [2, 3]. Typical bolus doses of phenylephrine range from 50 to 200 mCg repeated every 2 to 5 minutes to achieve hemodynamic goals [2, 3].
Ephedrine is an indirect alpha and beta-1 receptor agonist that is a popular choice in the OR due to its rapid onset (1 minute) and extended duration of action (60 minutes) [2, 3]. However, this longer duration of action may lead to overcorrection of hypotension or bradycardia (i.e. hypertension, tachycardia), so its use in the ED is not recommended [2].
Push-dose norepinephrine has recently gained attention in the anesthesia literature due to its lower tendency to cause tachycardia or reduce cardiac output [9]. Norepinephrine is a potent alpha agonist with modest beta agonist properties that induces vasoconstriction, increases blood pressure, and increases myocardial contractility with lower risk of tachycardia [1, 10]. Push-dose norepinephrine has a rapid onset (<1 minute) and short duration of action (1-2 minutes) [10]. The optimal dosing regimen has not been determined, although dosing used during anesthesia has ranged from 3-12 mcg every 1 to 2 minutes based on response [9-11]. However, evidence to support norepinephrine as a push dose pressor in the ED is lacking.
Properties and indications of epinephrine and phenylephrine are summarized below (Table 1). Choice of vasopressor is dependent upon the patient’s clinical presentation. For example, if a patient has hypotension with bradycardia, an agent with vasoconstrictive and chronotropic properties may be preferred (i.e. epinephrine) [2, 3]. If a patient has hypotension without bradycardia, phenylephrine may be preferred [2, 3]. Patients with cardiogenic shock present a more challenging clinical scenario. Epinephrine use as a continuous infusion has been associated with higher incidence of refractory shock after acute myocardial infarction (AMI) compared to norepinephrine infusion [12]. However, this has not been observed after push-dose use alone. Phenylephrine may decrease cardiac output due to its vasoconstrictive effects, which is undesirable in patients with compromised cardiac output (i.e. cardiogenic shock) [10]. Based on mechanism of action alone, epinephrine would be a better choice in these patients, especially in patients with concurrent bradycardia. However, providers may want to limit push-dose epinephrine by using it as a bridge to norepinephrine continuous infusion (e.g. 1-2 push-doses of epinephrine while waiting for preparation of norepinephrine drip).
Table 1. Comparison of Push-Dose Vasopressors

*Note: continuous infusion of epinephrine linked to higher incidence of refractory shock and lactic acidosis versus norepinephrine in patients with cardiogenic shock post myocardial infarction [12].
Evidence for Use
There is currently limited research evaluating the efficacy and safety of push-dose vasopressors in the ED or ICU setting. Evidence is currently limited to case series and retrospective studies. Results from prospective, randomized controlled trials are not available. Below we evaluate some of the most recent evidence discussing push-dose pressor use outside the OR.
Panchal et al. evaluated the use of push-dose phenylephrine for peri-intubation hypotension in the ED [8]. Adult patients who were hypotensive (SBP <90 mmHg) during the peri-intubation period (30 minutes before and after intubation) and received push-dose phenylephrine were included [8]. Twenty patients were included, with a mean time to administration of 4±13 minutes post intubation. Sixty-five percent (13/20) received multiple doses of phenylephrine, and 70% (14/20) received subsequent continuous vasopressor infusion [8]. Phenylephrine successfully increased SBP and DBP (mean SBP from 73 to 93 mmHg, mean DBP from 42 to 52 mmHg; p<0.05), with no appreciable changes in HR [8]. The authors concluded the use of push-dose phenylephrine was most commonly used as a bridge to vasopressor infusions or aggressive fluid resuscitation [8].
Gottlieb described a case series of push-dose epinephrine in post-cardiac arrest patients with ROSC and hypotension [4]. Three patient cases were presented in which push-dose epinephrine (10 mCg every 1-2 minutes for 8-12 doses) was given for hypotension refractory to IV fluid administration [4]. Epinephrine improved blood pressure in all cases; however, continuous vasopressors (e.g. norepinephrine) were required in all patients [4].
Rotando et al. retrospectively analyzed the use of push-dose phenylephrine and ephedrine in hypotensive patients outside of the OR [7]. They evaluated 155 push-dose events in 146 patients, with most doses given during the peri-intubation period (57.3%) [7]. Most patients received treatment in the surgical ICU or medical ICU (combined 78% of use) [7]. The mean doses of phenylephrine and ephedrine were 147±68.8 mCg and 14.2±8.5 mg respectively, with most patients (75%) receiving one dose [7]. The mean observed change in SBP was 26 mmHg (32.5% change), DBP was 13 mmHg (27.2% change), and HR was 6 bpm (6.4% change) [7]. Only 28% of patients required continuous vasopressor infusion [7]. Seventeen patients (11.6%) were identified as having an adverse event to push-dose vasopressors (SBP increase >100%, HR increase >30%, or dysrhythmia) and 13 medication dosing errors occurred (phenylephrine >200 mCg or ephedrine >25 mg) [7]. Overall, the authors concluded push-dose vasopressors are effective in resolving hypotension but are associated with adverse events and frequent medication errors [7].
Swenson et al. retrospectively reviewed records of all patients that received push-dose phenylephrine in the ED [6]. Changes in hemodynamics (e.g. MAP, SBP, DBP, HR) were used to assess efficacy and safety [6]. Doses ranged from 10-500 mCg and 45% of patients received multiple doses[6]. Fifty nine percent required additional vasopressors or inotropes (e.g. norepinephrine, epinephrine, dopamine) [6]. Eighty percent of patients received push-doses for medical indications (e.g. sepsis, respiratory distress/failure, cardiac arrest) and the remainder received doses for trauma-induced hypotension (hemorrhagic or neurogenic shock)[6]. Mean increase in MAP ranged from 4-12 mmHg while mean change in HR ranged from -2.4 to +2.2 depending on dose [6]. Only 3% of patients developed hypertension or bradycardia within 30 minutes of push-dose administration [6]. None of these adverse effects resulted in apparent harm [6]. The authors concluded that push-dose phenylephrine does not appear to cause harm in hypotensive ED patients [6].
Schwartz et al. retrospectively reviewed records of adults that received push-dose phenylephrine in the ED [13]. Objectives were to assess the need for continuous vasopressor infusion within 30 minutes of push-dose administration and the impact of early preload expansion with IV crystalloid [13]. Phenylephrine doses ranged from 100-200 mCg and 53.4% received multiple doses [13]. Most patients had septic shock (45.2%) and use was most often for peri-intubation hypotension (71.2%). Forty six and a half percent required continuous vasopressors (mostly norepinephrine)[13]. Patients that received less than 30 mL/kg of IV fluid required more doses of phenylephrine (2.3 vs. 1.5; p=0.01) [13]. Fifteen patients (20.5%) developed adverse events within one hour after phenylephrine, which included bradycardia (HR<60 bpm), reactive hypertension (SBP>180 mmHg), and ventricular tachycardia (HR>100 bpm) with frequencies of 9.6%, 8.2%, and 2.7%, respectively [13]. The authors concluded that further study to assess appropriateness, efficacy, and safety of push-dose phenylephrine is needed [13].
Table 2. Studies Assessing Efficacy and Safety of Push-Dose Vasopressors outside the OR

SBP: systolic blood pressure, DBP: diastolic blood pressure, HR: heart rate, MAP: mean arterial pressure, SICU: surgical ICU, MICU: medical ICU, ICU: intensive care unit, ADE: adverse drug events. Note: units for are mmHg for SBP, DBP, or MAP and beats per minute for HR.
Preparation [2, 3]
Because push-doses vasopressors are not available commercially, providers that decide to use them will need to prepare them at bedside. This generally involves diluting commercially available products (e.g. epinephrine syringes used for ACLS). Bedside mixing is a risky process that can lead to dosing errors and patient harm. We highly recommend that organizations develop a standardized process for naming, dosing, ordering, preparing, and administering these agents. Standardization is even more important if your institution utilizes different epinephrine preparation methods (e.g. “dirty epi drip”). Confusion leading to errors is likely if push-dose epinephrine, epinephrine for cardiac arrest, epinephrine continuous infusion, “dirty epi” infusion, and epinephrine for anaphylaxis are all orderable within your ED. If possible, consider limiting the amount of orderable epinephrine products.
If your organization currently does not have a standardized process for preparation of push-dose pressors, consider the steps below:
Epinephrine
-
- Dose: 5-20 mCg
- Target syringe concentration: 10 mCg/mL
- Items needed:
- Epinephrine 1 mg/10 mL syringe (0.1 mg/mL)
- This is the syringe commonly used for ACLS
- 0.9% sodium chloride (NS) vial or bag
- Due to potential for mislabeling, “flush” syringes are NOT recommended
- 10 mL syringe
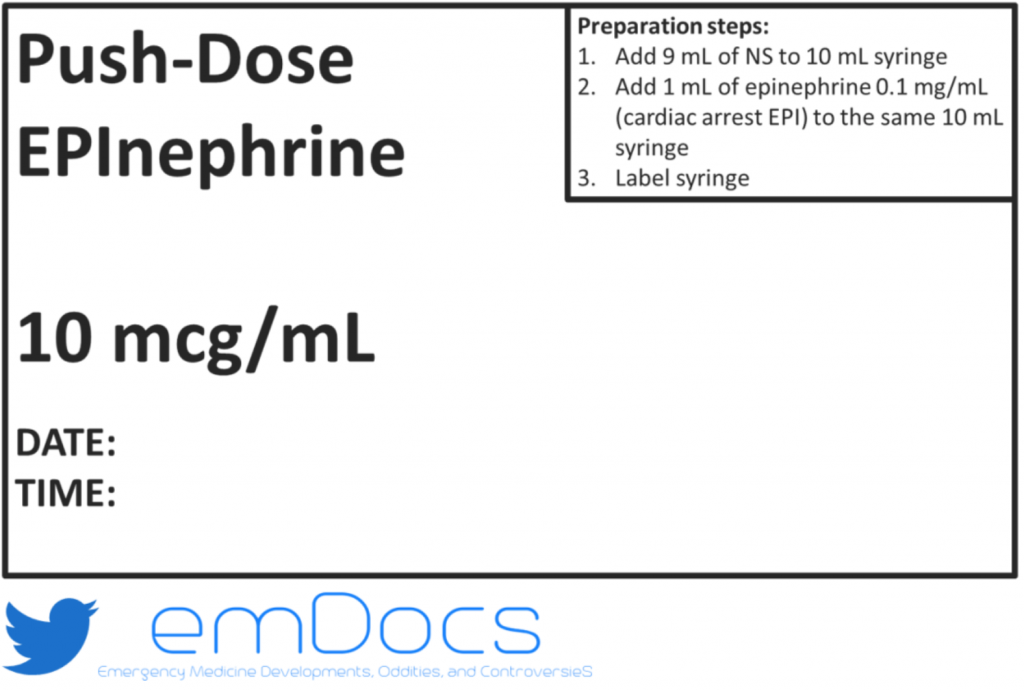
- Medication label for “Epinephrine 10 mCg/mL” (see Figure 1)
- Epinephrine 1 mg/10 mL syringe (0.1 mg/mL)
- Preparation steps:
- Add 9 mL of NS to 10 mL syringe
- Add 1 mL of epinephrine 0.1 mg/mL to the same 10 mL syringe
- Label syringe
- Each 1 mL now contains 10 mCg of epinephrine (10 mCg/mL)
- 0.5 mL = 5 mCg
- 1 mL = 10 mCg
- 2 mL = 20 mCg
- Notes:
- 1 mg = 1000 mCg
- There are other methods for preparing the desired syringe concentration; however, the above method is one of the simplest
Phenylephrine
-
- Dose: 50-200 mCg
- Target syringe concentration: 100 mCg/mL
- Items needed:
- Phenylephrine 10 mg/mL vial
- These are commonly used when preparing continuous infusions
- NS 100 mL bag
- 10 mL syringe
- Medication label for “Phenylephrine 100 mCg/mL” (see Figure 2)
- Phenylephrine 10 mg/mL vial
- Preparation steps
- Use syringe to remove 1 mL from phenylephrine 10 mg/mL vial
- Add this 1 mL of phenylephrine to 100 mL NS bag
- Remove 10 mL from this NS bag containing phenylephrine by using the 10 mL syringe
- Label syringe
- Each 1 mL now contains 100 mCg of phenylephrine (100 mCg/mL)
- 0.5 mL = 50 mCg
- 1 mL = 100 mCg
- 2 mL = 200 mCg
- Notes:
- 1 mg = 1000 mCg
- There are other methods for preparing the desired syringe concentration; however, the above method is one of the simplest

Key considerations
-
- Use extreme caution when preparing these medications due to high risk of error
- Standardize concentrations, dosing, and who can administer
- Use the same names for products
- Ensure clear labeling
- Educate staff on use
- Ensure items needed are easily accessible yet secure
- We HIGHLY recommend using pre-packaged products prepared in the pharmacy
- If available, consider requesting these products for storage in your ED
- Use extreme caution when preparing these medications due to high risk of error
What happens if you give too much?
Because preparation of push-dose vasopressors typically involves multiple steps in a less than ideal work environment (i.e. a busy ED), there is a chance of unintentional medication overdose. Rotando et al. reported that dosing errors (>200 mCg per dose) occurred in 10.3% (12/104) of patients receiving push-dose phenylephrine [7]. One of these patients received 1000 mCg (10 mL of a 10 mCg/mL syringe) and developed SBP >300 mmHg requiring antihypertensive treatment [7]. Notably, harm was not described in the other 11 patients affected by dosing errors [7]. Preparation steps recommended above should ideally decrease the likelihood of this type of error; however, error is still possible. Providers using push-dose vasopressors should be prepared to manage unintentional overdose.
Currently, there are no guidelines discussing management after unintentional push-dose vasopressor overdose. Based on mechanism of action of these agents, tachycardia, hypertension, and reflexive bradycardia are the most likely effects [2, 3]. Arrhythmias (atrial or ventricular), limb ischemia, hypertension leading cerebrovascular events, metabolic acidemia, and lactic acidosis are more likely in patients receiving continuous infusions; however, they may develop after extreme overdose of push-doses [14]. Because epinephrine and phenylephrine have short half-lives, their adverse effects should be short lived (e.g. <30 minutes) [2, 3]. Studies evaluating push-dose adverse effects typically monitored these effects for up to 30 minutes after dose administration [6, 7]. If effects last longer than 30 minutes or if they lead to serious harm (e.g. organ ischemia), the administration of short-acting reversal agents (e.g. esmolol, nitroglycerin) should be considered. Reversal agents with longer durations of action may lead to hypotension after the push-dose agents are fully metabolized and eliminated.
Case Resolution
You recall that push-dose phenylephrine or epinephrine can be used for patients requiring rapid normalization of hemodynamic parameters. Because of the patient’s hypotension and bradycardia, you decide that epinephrine would be an ideal push-dose agent. You ask the nurse, “Do we have any push-dose epinephrine syringes?” He quickly runs to the medication cabinet and returns with two syringes- epinephrine 0.1 mg/mL (1 mg/10 mL) and epinephrine 10 mCg/mL. You realize that the 10 mCg/mL syringe is the appropriate push-dose product (i.e. it is more diluted) and the 0.1 mg/mL is typically for patients in cardiac arrest, although it could be used to compound a push-dose syringe. You instruct the nurse to give 10 mcg (1 mL) of epinephrine from the 10 mCg/mL syringe. The patient’s blood pressure and heart quickly increase to 110/70 and 80 bpm, respectively. The cardiologist feels comfortable taking the patient to the cath lab, but asks if she can take the epinephrine 10 mCg/mL syringe in case the patient requires it again. The nurse hands her the syringe and they rush to the cath lab.
Two days later, you see the same cardiologist in the cafeteria and ask how the patient that received the push-dose epinephrine is doing. She states the patient had an inferior MI and was successfully stented. He only needed one more dose of epinephrine 10 mCg while in the cath lab. He did require norepinephrine while receiving therapeutic hypothermia in the cardiac ICU; however, he started waking up yesterday and is now off vasopressors. He will probably be extubated today.
Great work ED team!
Take Home Points
- Due to their rapid onset and short duration of action, push-dose epinephrine and phenylephrine can be considered for patients with spontaneous circulation requiring rapid normalization of hemodynamic parameters (e.g. SBP, DBP, MAP, HR).
- Phenylephrine is generally best for patients with hypotension without bradycardia.
- Epinephrine is generally best for patients with hypotension and bradycardia.
- With the exception of procedure-related or medication-induced hypotension or bradycardia, push-dose pressors generally do not resolve the underlying clinical problem (e.g. sepsis, MI, hemorrhage).
- Studies have reported that 28-70% of patients require continuous infusion of vasoactive agents (e.g. norepinephrine) after receiving push-dose pressors.
- Limited evidence shows that push-dose pressors can increase SBP and DBP 10-20 mmHg within minutes.
- Push-dose pressors are typically dosed as phenylephrine 50-200 mCg every 2-5 minutes and epinephrine 5-20 mCg every 2-5 minutes to hemodynamic goal (e.g. MAP>65 mmHg)
- Push-dose pressors do not eliminate the need for IV fluids or blood products.
- If you choose to use push-dose pressors in your ED, ensure they are used as safely as possible.
- Hypertension, tachycardia, or reflex bradycardia may develop up to 30 minutes after administration of recommended doses.
- If serious adverse events develop after administration (e.g. severe hypertension with organ ischemia), consider short-acting antihypertensive agents (e.g. esmolol, nitroglycerin).
References
- Overgaard C.B. et al. Inotropes and vasopressors: review of physiology and clinical use in cardiovascular disease. Circulation 2008;118:1047-1056.
- Holden D. et al. Safety Considerations and Guideline-Based Safe Use Recommendations for “Bolus-Dose” Vasopressors in the Emergency Department. Ann Emerg Med 2018;71(1): 83-92.
- Tilton L.J. et al. Utility of Push-Dose Vasopressors for Temporary Treatment of Hypotension in the Emergency Department. J Emerg Nurs 2016;42(3):279-81.
- Gottlieb M. Bolus dose of epinephrine for refractory post-arrest hypotension. CJEM2018;20(S2):S9-13.
- Selde W. Push dose epinephrine: a temporizing measure for drugs that have the side effect of hypotension. Journal of Emergency Medical Services 2014;39(9):62-3.
- Swenson K. et al. Safety of bolus-dose phenylephrine for hypotensive emergency department patients. American Journal of Emergency Medicine 2018;36:1802-1806.
- Rotando A. et al. Push dose pressors: Experience in critically ill patients outside of the operating room. Am J Emerg Med 2019;37(3):494-498.
- Panchal A.R. et al. Efficacy of Bolus-dose Phenylephrine for Peri-intubation Hypotension. J Emerg Med 2015;49(4):488-94.
- Wang X. et al. A Comparative Study of Bolus Norepinephrine, Phenylephrine, and Ephedrine for the Treatment of Maternal Hypotension in Parturients with Preeclampsia During Cesarean Delivery Under Spinal Anesthesia. Med Sci Monit 2019;25:1093-1101.
- Wang X. et al. The Efficacy and Safety of Norepinephrine and Its Feasibility as a Replacement for Phenylephrine to Manage Maternal Hypotension during Elective Cesarean Delivery under Spinal Anesthesia. Biomed Res Int 2018; 2018:1869189.
- Hassani V. et al. Comparison of Ephedrine vs. Norepinephrine in Treating Anesthesia-Induced Hypotension in Hypertensive Patients: Randomized Double-Blinded Study. Anesth Pain Med 2018;8(4):e79626.
- Levy B. et al. Epinephrine Versus Norepinephrine for Cardiogenic Shock After Acute Myocardial Infarction. J Am Coll Cardiol 2018;72(2):173-182.
- Schwartz M.B. et al. The impact of push-dose phenylephrine use on subsequent preload expansion in the ED setting. American Journal of Emergency Medicine 2016;34:2419-2422.
- Stratton L. et al. Vasopressors and inotropes in sepsis. Emerg Med Clin North Am 2017;35:75-91.
Related emDOCs content- http://www.emdocs.net/push-dose-pressors/
Other related content-https://www.foamfrat.com/single-post/2017/08/11/Ahh-push-it-push-it-real-good








3 thoughts on “Push-Dose Vasopressors: An Update for 2019”
Not to mention it has utility during EMS critical care transport (https://www.ncbi.nlm.nih.gov/pubmed/30808241). We are also currently working on designing a multicenter trial on using push-dose epinephrine to manage hypotension in the EMS/critical care transport setting that will hopefully provide more of an evidence base for its use in Emergency Medicine/EMS!
Pingback: Quiz 34, 10th of May 2019
Pingback: Shifting Paradigms In Prehospital Vasoactive Therapy: A Case For Push Dose Vasopressors In Prehospital Protocols - JEMS