Author: Kristen Kann, MD (EM Staff Physician, SAUSHEC, USAF) // Edited by: Brit Long, MD (@long_brit, EM Chief Resident at SAUSHEC, USAF) and Alex Koyfman, MD (@EMHighAK)
An 18 year-old male recently diagnosed with infectious mononucleosis by Monospot presents to the Emergency Department complaining of three days of left upper quadrant pain. He denies any recent trauma or participation in contact sports. His review of systems is otherwise negative, with no fever, nausea, rashes, or other complaints noted. He appears mildly uncomfortable on exam but otherwise is in no acute distress. His initial vital signs include BP 119/55, HR 97, RR 16, T 98.8F, Sat 99%, and a pain scale of 6/10. His lungs and heart are normal, but his abdominal exam is significant for moderate left upper quadrant tenderness to palpation without rebound or guarding. No organomegaly is appreciated on exam. The remainder of his physical exam is unremarkable, including skin and lymph nodes.
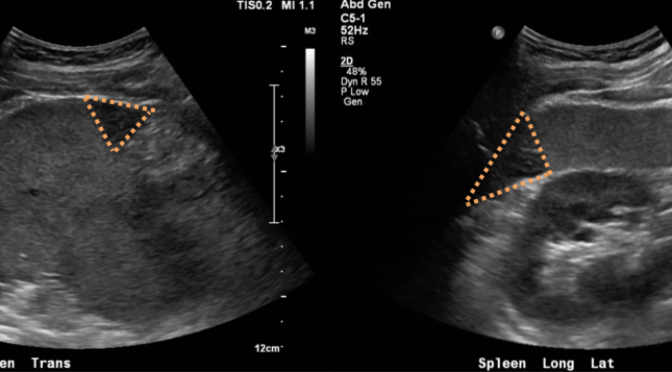
A review of recent workup reveals a splenic ultrasound three days prior to the patient’s presentation, which he reports coincided with the onset of the left upper quadrant pain. The ultrasound was significant for multiple hypodensities in the spleen and splenomegaly.
BACKGROUND
The spleen is a large reticuloendothelial organ in the left upper quadrant that functions to filter red blood cells, produce antibodies (specifically IgM), and remove antibody-coated bacteria from the bloodstream.
The spleen can become infarcted when flow from the splenic artery or one of its branches is interrupted, causing hypoperfusion of splenic segments and eventual tissue death. Causes of splenic infarction can be broken down into three main categories: hematologic conditions that result in splenomegaly, systemic thromboembolic conditions, and trauma.
Splenomegaly occurs with splenic enlargement. The differential for splenomegaly is very large and includes diseases that increase demand for splenic filtration (autoimmune hemolytic anemia, polycythemia vera, spherocytosis, early sickle cell anemia, thalassemias), certain infectious diseases (infectious mononucleosis, AIDS, CMV, and malaria, among others), and splenic infiltration (sarcoidosis, myelofibrosis, metastatic disease, amyloidosis, leukemias, and lymphomas). Infectious mononucleosis was previously diagnosed in this patient and was his only known risk factor. Splenic infarction has been reported as a rare complication of infectious mononucleosis/Epstein Barr Virus infection, but the incidence is unknown.
The vascular network of the spleen can also become the site of thromboembolic disease, such as in the case of malignancy, antiphospholipid antibody syndrome, infectious endocarditis, atrial fibrillation, and sickle cell disease. Interestingly, splenic infarction has been reported in patients with sickle cell trait who were otherwise asymptomatic but presented with left upper quadrant pain after heavy exertion at altitude.
Trauma that affects the blood flow to the spleen, either directly or as a result of compression (ex. splenic hematomas) can also cause splenic infarction. In addition, the Emergency Physician may encounter a patient who has symptomatic splenic infarction after splenic artery embolization.
Rarely, the splenic artery can become torsed in “wandering spleen syndrome,” a rare condition seen in children and young adults in which the spleen is more mobile than usual, leading to infarction of the entire spleen.
SIGNS/SYMPTOMS
Patients with splenic infarction can present in a myriad of ways. Up to 30% may be completely asymptomatic, especially those with nonmalignant hematologic conditions. The most common signs and symptoms in patients with complaints include left sided abdominal pain, fever, nausea/vomiting, elevated LDH, and leukocytosis. While abdominal tenderness to palpation is relatively easy to elicit, splenomegaly is notoriously difficult to appreciate on physical exam. One study compared percussion and palpation by physicians with the gold standard of ultrasonographic measurement and found palpation to have a sensitivity of 56-71% for splenomegaly, with similar results for percussion. Thus, the Emergency Physician should not rely on physical exam alone to exclude splenomegaly, and certainly not to exclude splenic infarction, as there are many causes that can occur in normal or even shrunken spleens (such as advanced sickle cell anemia).
WORK UP
For a patient in whom you suspect splenic infarction, the basic work up should likely include a complete blood count and LDH, with a consideration for peripheral blood smears and manual differentials based on the suspicion for underlying causes. Initial imaging can include ultrasound or computed tomography. Ultrasound has the benefit of being radiation free, relatively fast, and being able to reliably exclude splenomegaly, though some splenic infarcts may be hard to visualize if they are very small and/or more centrally located in the abdomen. Computed tomography, though it does involve an IV dye load and radiation, has the advantage of visualizing the entire spleen while also showing the rest of the abdominal organs in the cases in which the differential is broad.
For the vast majority of splenic infarctions, the main concerns for the Emergency Physician are the determination of the underlying cause and providing proper disposition. If there is no obvious cause already known, but the patient is stable, pain is well controlled, and follow up can be reliably obtained, most patients can be discharged home with outpatient follow up, either with their primary care physician or a hematologist. If the patient is hemodynamically unstable, or if there is evidence of splenic rupture or abscess associated with the infarction, then consultation with Surgery or Interventional Radiology for further treatment and admission should be obtained. While many cases of splenic rupture can be managed non-operatively, the patient will require close observation and consideration for splenic artery embolization or splenectomy. Splenic abscess will require antibiotics as well as drainage or splenectomy. In any patient with a significant portion of their spleen affected by infarction, resultant functional hyposplenia should be anticipated, and the patient will need follow up to provide the appropriate vaccinations and monitoring.
CASE CONCLUSION
The Emergency Department workup for this patient consisted of a complete blood count, a comprehensive metabolic profile, and coagulation studies in addition to a CT scan of the abdomen with IV contrast, as requested by radiology. A CT was selected to better characterize the total number and size of the lesions and to evaluate for any complications such as abscess or rupture. Laboratory work up was all within normal limits, and the CT scan revealed multiple peripheral small wedge-shaped hypodensities within the spleen measuring up to 1.9 cm. The patient remained hemodynamically stable throughout his ED stay, and his pain was well controlled. He was counseled to continue to avoid contact sports and to return to the Emergency Department for any increase in pain, fever, or other concerns. He was discharged with Hematology follow up. His clinical course remained unremarkable, and given the large portion of unaffected splenic tissue, he did not require any additional vaccines.
SUMMARY
Splenic infarction is a rare complication of infectious mononucleosis, and a rare disease in general, but should be considered in the ED differential of patients with left upper quadrant pain. Special consideration for this diagnosis should be given to those patients with a history of conditions predisposing to splenomegaly, a history of thromboembolic disease, and in those with a history of abdominal trauma. Management for most patients will consist of supportive case and avoidance of splenic injury (no contact sports), while some patients will require admission and consideration for splenectomy, especially if splenic abscess or splenic rupture develop.
References / Further Reading
-Harrison’s Principles of Internal Medicine 19ed
-Tintinalli’s Emergency Medicine 8ed
-Sabiston Textbook of Surgery
-The clinical spectrum of splenic infarction.
Nores M, Phillips EH, Morgenstern L, Hiatt JR
Am Surg. 1998;64(2):182.
PMID: 9486895
-Splenic infarction: an update on William Osler’s observations.
Lawrence YR, Pokroy R, Berlowitz D, Aharoni D, Hain D, Breuer GS
Isr Med Assoc J. 2010;12(6):362.
PMID: 20928991
-Splenic infarction: 10 years of experience.
Antopolsky M, Hiller N, Salameh S, Goldshtein B, Stalnikowicz et al .
Am J Emerg Med 2009;27:262–5.







1 thought on “Splenic Infarction in Mononucleosis: Pearls and Pitfalls”
Pingback: PEM Review 018: UTIs // EYE EXAMS // SPLEIC INFARCTS // RASHES // FOREIGN BODIES | PEMgeek.com: #FOAMed highlights from the world of Paediatric Emergency Medicine