Authors: Haley Dusek, MD (Emergency Medicine Resident, Carolinas Medical Center); Erik Fisher, MD (Emergency Medicine Attending/Medical Toxicologist, Carolinas Medical Center) // Reviewed by: Anthony Spadaro, MD (@TSpadaro91, Medical Toxicology Fellow, Rutgers New Jersey Medical School, Newark, NJ); James Dazhe Cao, MD (@JamesCaoMD, Associate Professor of EM, Medical Toxicology, UT Southwestern Medical Center, Dallas, TX); Alex Koyfman, MD (@EMHighAK); and Brit Long, MD (@long_brit)
Case:
A 27-year-old woman presents to the emergency department (ED) with altered mental status. A partner at bedside reports recent depressed mood, abdominal pain, and vomiting yesterday. The patient woke up confused this morning, and has had a worsening mental status throughout the day today. On arrival to the ED the patient’s initial vital signs are temperature 38.5°C, BP 102/48, HR 106, RR 20. The exam is notable for altered mentation and grimace with palpation of the abdomen diffusely. Initial labs include a venous blood gas (VBG) with pH 7.05, lactate of 10 mmol/L, anion gap of 20, and a glucose of 42 mg/dL. A chest x-ray does not demonstrate any acute abnormalities, but radiopaque tablets are incidentally noted in the abdomen. The patient’s partner reports that the patient takes an iron supplement (formulation: ferrous sulfate, 325 mg tablets, 20% elemental iron).
Questions:
- What is the expected toxic dose of iron?
- What is the typical clinical course of iron toxicity?
- What is the role of radiography in acute iron ingestion?
- What are the indications for treatment with deferoxamine?
Background:
- Iron (Fe) is a chemical element, classified as a transition metal, and commonly found in homes as a nutritional supplement.
- Iron is used for treatment and prevention of iron-deficiency anemia.
- Historically, iron toxicity and exposure affected children in unintentional overdose disproportionately. In the late 1990s, iron was the leading cause of poisoning deaths reported to poison control centers for children less than 6 years of age.1
- The incidence of iron overdose and iron ingestion related deaths has significantly decreased over time, likely attributable to federal regulation. In 1997, the Food and Drug Administration (FDA) mandated unit-dose packaging for all iron-containing products with more than 30 milligrams of elemental iron.2 This requirement was ultimately removed in 2003, however iron related exposures and deaths have stayed low.
- The oral bioavailability of inorganic iron is < 10%; ferrous iron (Fe2+) is better absorbed than ferric iron (Fe3+).
- Iron is primarily absorbed in the duodenum.
- Ferrous iron is transported into enterocytes by membrane proton-coupled metal transporter.
- Ferrous iron is oxidized to ferric iron within enterocytes.
- Ferric iron is transported from enterocytes into circulation by carrier protein, transferrin.3
- About 2/3 of the body’s iron is found in hemoglobin stores.
- Iron is a potent catalyst for hydroxyl radicals and an inducer of oxidant stress.
- This results in direct oxidative damage to gastrointestinal (GI) tract epithelium by iron-induced reactive oxygen species, compromise of the enterocyte barrier, and allows iron ions to be released into systemic circulation.4
- Iron concentrations are regulated by restriction of GI uptake and mucosal sloughing; there is no physiologic mechanism for iron removal following absorption.3
- Toxicity is related to the amount of elemental iron ingested. However non-ionic iron formulations such as carbonyl iron appear to be less toxic than iron salts such as ferrous fumarate despite higher elemental iron content.1
- Commercially available formulations of iron have varying elemental components.1
Table 1: Iron content of various preparations.

- Toxic effects begin at doses between 10-20 milligram/kilogram of elemental iron.1
- Moderate toxicity: 20-60 mg/kg elemental iron.5
- Severe toxicity: >60 mg/kg elemental iron.5
- Toxicologic effects are primarily due to free radical formation and direct cellular injury.5
- Oxidative stress on GI epithelium causes the initial symptoms of iron toxicity (GI upset, vomiting, mucosal irritation, and bleeding).
- Free iron enters the electron transport chain and uncouples oxidative phosphorylation which leads to anaerobic metabolism, producing lactate, and an anion gap metabolic acidosis.
- Hepatotoxicity is the result of large volume deposition of iron stores to the liver from portal circulation.
- Coagulopathy can result from both iron causing inhibition of thrombin formation and an effect of hepatotoxicity.
- Myocardial dysfunction results from direct negative inotropic effects and myocardial deposition of iron.
- Hypotension can be multifactorial secondary to volume depletion, vasodilation, and negative inotropy.
Clinical Presentation:
- Stage 1 (0-6 hours) Local Toxicity1:
- GI symptoms predominate (abdominal pain, nausea, vomiting, and diarrhea).
- Typically presents in the first few hours following ingestion.
- Children without vomiting within 6 hours of iron ingestion will almost never have significant toxic effects.6
- Can see subsequent electrolyte disturbances and dehydration related to severity of GI symptoms.
- In severe toxicity, hematemesis, melena, or hematochezia may occur.
- Stage 2 (6-24 hours) “Latent” Period1:
- Improvement in GI symptoms specifically. Be wary of this stage.
- This stage does not always occur.6
- Typically described as the period between resolution of GI symptoms and the development of clinically apparent systemic toxicity;
- Patients at this stage may be lethargic, have tachycardia, or have a metabolic acidosis on laboratory evaluation.
- This stage is not truly quiescent as cellular toxicity progresses.
- Stage 3 (timing variable) Shock1:
- Can occur within hours for massive ingestion, but may occur over a longer time course.
- Characterized by hypovolemia, vasodilation, reduced cardiac output, hyperventilation, elevated temperature, seizure, coma, and cardiovascular collapse.
- Stage 4 (2-5 days after ingestion) Hepatic Stage5:
- Can have increased aminotransferase levels, hypoglycemia, and coagulopathy.
- Can progress to hepatic failure.
- Stage 5 (2-8 weeks after ingestion) Delayed Sequelae5:
- Presents as gastric outlet obstruction due to scarring and strictures from direct GI injury and corrosion of pyloric mucosa.
- It is rare for delayed sequelae to occur in the absence of severe toxicity in the earlier stages.
Diagnosis:
- Iron toxicity is primarily a clinical diagnosis.
- Focus on thorough history, specific formulation ingested, review of available medications in the home to screen for possible co-ingestions, and physical exam.
- Labs to obtain: Complete blood count (CBC), basic metabolic panel (BMP), liver function tests (LFTs), coagulation panel, serum glucose, VBG, and on arrival if time of ingestion is unknown, or 4 hours following a known ingestion time.
- Consider acetaminophen and aspirin level if there is concern for intentional ingestion or self-harm.
- Significant clinical toxicity is uncommon with serum iron concentration less than 300 μg/dL.6
- Severe toxicity and shock are typically seen with serum iron concentrations above 500 μg/dL and serum iron concentrations above 1000 μg/dL are associated with significant mortality.1
- Obtain a single view abdominal x-ray.
- Ferrous sulfate tablets are radiopaque and can be visualized on radiographs, however not all preparations are radiopaque (pediatric chewable and liquid preparations).
- If large number of tablets are visualized on abdominal x-ray, it can help guide GI decontamination decisions.6
- Absence of visualized tablets on x-ray does not exclude iron ingestion.7
- Workup other than serum iron concentration at 4 hours after ingestion not shown to accurately predict clinical outcomes or severity of toxicity.8
- A white blood cell count (WBC) greater than 15,000/mm3, or a glucose greater than 150 mg/dL have been suggested to predict significant iron toxicity, but a normal WBC or glucose do not exclude iron toxicity.1
Management:
- Supportive care first and foremost.
- Basic assessment: airway, breathing, circulation.
- Consider intubation for patients with airway compromise, respiratory failure, altered mental status, or seizure.
- Aggressive fluid resuscitation as patients may be severely hypovolemic from GI symptoms.
- Antiemetics as needed.
- Consider GI decontamination with whole bowel irrigation (WBI).
- Although there is no clear outcome benefit, given limited other options for GI decontamination, consider WBI patients with severe toxicity, evidence of retained tablets in the GI tract by x-ray, or extended release formulations.9
- Typical dose: Polyethylene glycol (Go-Lytely™) 25 mL/kg/hr in small children and 1.5-2 L/hr in adults.9
- There is no role for activated charcoal as it does not adsorb iron.11
- Can consider endoscopy, or surgical evaluation if critically ill with known iron bezoar.5
- Orogastric lavage may also be considered for GI decontamination but likely to be limited by location, size of tablets, and operator familiarity.1
- The choice of GI decontamination should be made with toxicologist / poison control review and recommendation, and possibly including endoscopist input.
- Antidote:
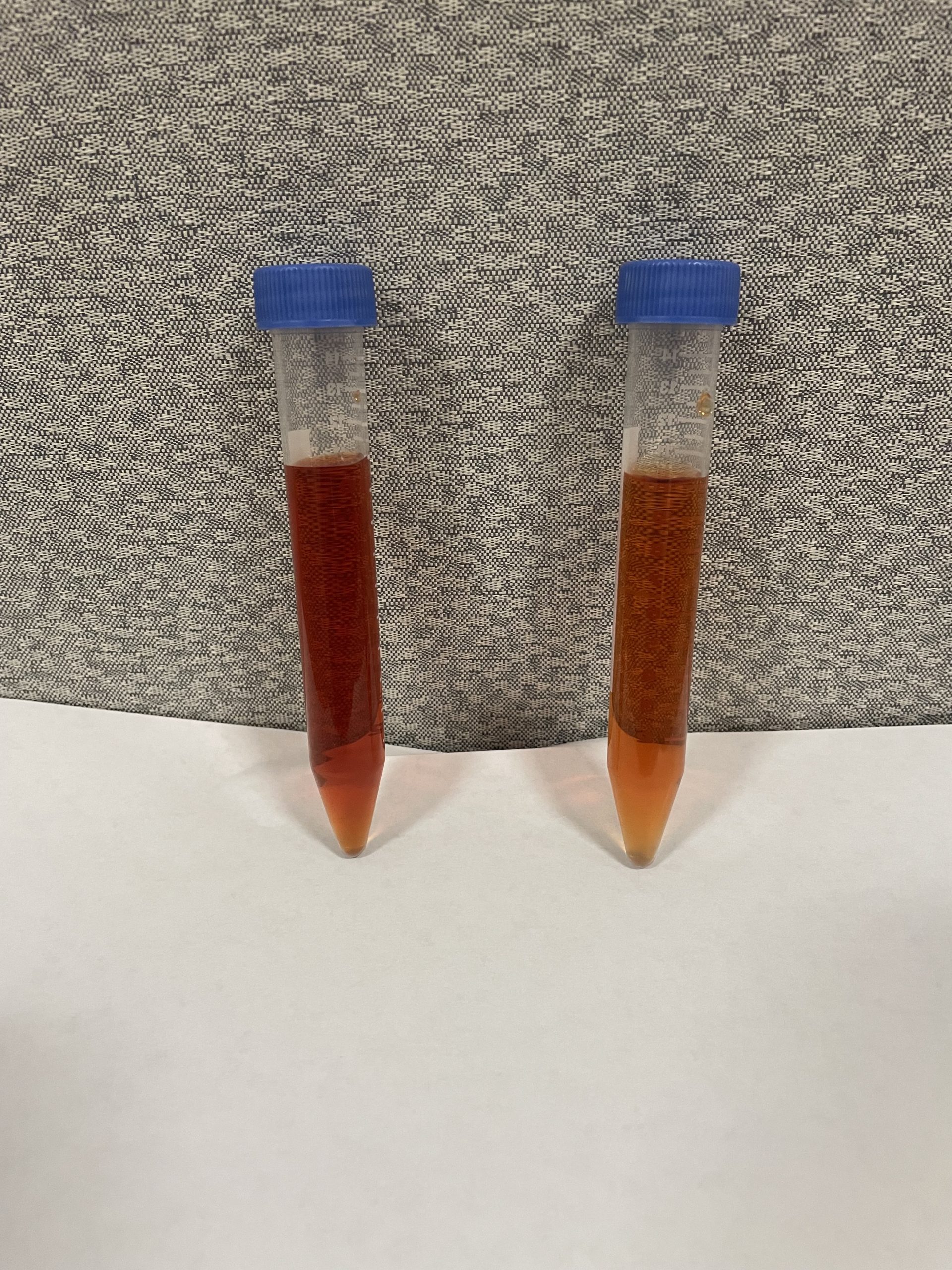
- Deferoxamine is a chelating agent derived from Streptomyces pilosus; binds free iron from plasma and iron inside of cells. Forms ferrioxamine complex which is renally excreted, may give urine a Vin rosé appearance (picture below).1
- Deferoxamine is safe in children. The exact risk of deferoxamine in pregnancy is unclear, although there are case reports of safe use in pregnant women and benefits likely outweigh risks in severe toxicity.
- 100 mg of deferoxamine binds 8.5 mg of elemental iron.1
- Indication: evidence of systemic toxicity including persistent emesis, metabolic acidosis, progressive symptoms, altered mental status, GI hemorrhage, or serum iron concentration greater than 500 μg/dL.1
- Infusion:
- Usual recommendation for starting dose: 5 mg/kg/hr.1,5,6
- Defuroxamine can be given intramuscularly but is most often given intravenously (IV).
- Can titrate up to maximum of 40 mg/kg/hr, although hypotension may limit dose of deferoxamine.10
- Maximum daily dose of 6-8g total of defuroxamine.1
- Consider increasing dose by 5 mg/kg/hr every 2-4 hours10 if:
- Vin rosé urine persists (ongoing chelation) – be aware of limitations including difficulty detecting color change and color change latency.5
- Severe metabolic acidosis persists
- Multi-system organ failure
- The endpoints of deferoxamine are less well defined but it can be weaned off as the patient is clinically improving, the anion gap resolves, and down-trending serum iron concentration.1
- Adverse reactions: Hypotension (usually rate of infusion related), anaphylactoid reaction, ALI/ARDS with prolonged infusions (> 24 hours), and increased risk of Yersinia1,10
- Hypotension: IV fluid resuscitation, norepinephrine, or other vasopressors as needed.
- Coagulopathy: Parenteral vitamin K and/or fresh frozen plasma (FFP) as clinically indicated.
- Blood transfusion for clinically significant blood loss.5
- Seizure: IV benzodiazepine first line, barbiturates as second line.
- Enhanced elimination:
- Some patients with severe renal impairment may require dialysis for removal of deferoxamine-iron complexes.5
- Consider exchange transfusion in addition to deferoxamine for serum iron concentrations greater than 1000 μg/dL, or those who clinically deteriorate despite supportive care and chelation.10
- Disposition:
- A medical toxicologist or local poison control center should be consulted for known or suspected iron ingestions.
- Intentional ingestions need evaluation at a medical facility regardless of dose.
- Unintentional ingestions > 40 mg/kg of elemental iron should be evaluated at a medical facility. 6,11
- Any ingestion with severe or persistent symptoms should be evaluated at a medical facility.
- Asymptomatic unintentional ingestions, or with 1 episode of emesis, and no further symptoms after 6-hour observation period can be discharged home.6
- Patients who receive deferoxamine, have significant metabolic abnormalities, or hypotension should be admitted to an intensive care unit (ICU).1
Picture 1: Vin rosé appearance of urine after treatment with deferoxamine.
Case Follow-up:
- The patient received a fluid resuscitation with 20 mL/kg bolus of normal saline. Based on x-ray findings, history, and systemic toxicity, an NG tube was placed, and whole bowel irrigation with polyethylene glycol was performed. The patient’s serum iron concentration resulted at 400 μg/dL. She was initiated on deferoxamine and admitted to the ICU.
Clinical Pearls:
- Iron toxicity can cause severe metabolic acidosis and end organ dysfunction due to uncoupling of oxidative phosphorylation, anaerobic metabolism, and direct toxicity of iron deposits in organs.
- Expect systemic toxicity with elemental iron ingestions of 20-60 mg/kg, or serum iron concentration greater than 300 μg/dL. Severe toxicity can occur with ingestion of greater than 60 mg/kg of elemental iron or serum iron concentration greater than 500 μg/dL.
- Obtain serum iron concentration at 4 hours after ingestion, if time of ingestion is known, otherwise obtain on arrival. Obtain an abdominal x-ray to evaluate tablet burden and to guide GI decontamination.
- Consider GI decontamination if tablets are visualized on x-ray or if severe toxicity is present. Indications for treatment with deferoxamine: serum concentration greater than 500 μg/dL, metabolic acidosis, persistent GI symptoms, altered mental status, and GI hemorrhage.
References:
- Perrone J. Iron. In: Nelson LS, Howland M, Lewin NA, Smith SW, Goldfrank LR, Hoffman RS. eds. Goldfrank’s Toxicologic Emergencies, 11e. McGraw Hill; 2019.
- Tenenbein M. Unit-dose packaging of iron supplements and reduction of iron poisoning in young children. Arch Pediatr Adolesc Med. 2005 Jun;159(6):557-60. doi: 10.1001/archpedi.159.6.557. PMID: 15939855.
- McDermid JM, Lönnerdal B. Iron. Adv Nutr. 2012;3(4):532-533. Published 2012 Jul 1. doi:10.3945/an.112.002261.
- Anderson GJ, Wang F. Essential but toxic: controlling the flux of iron in the body. Clin Exp Pharmacol Physiol. 2012 Aug;39(8):719-24. doi: 10.1111/j.1440-1681.2011.05661.x. PMID: 22211782.
- Hernandez SH, Nelson LS. Iron. In: Tintinalli JE, Stapczynski J, Ma O, Yealy DM, Meckler GD, Cline DM. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e. McGraw Hill; 2016.
- Chang, T. P. & Rangan, C. (2011). Iron Poisoning: A Literature-Based Review of Epidemiology, Diagnosis, and Management. Pediatric Emergency Care, 27 (10), 978-985. doi: 10.1097/PEC.0b013e3182302604.
- Hosking CS. Radiology in the management of acute iron poisoning. Med J Aust. 1969;1(11):576-579. doi:10.5694/j.1326-5377.1969.tb92297.x
- Chyka PA, Butler AY. Assessment of acute iron poisoning by laboratory and clinical observations. Am J Emerg Med. 1993;11:99-103. doi:10.1016/0735-6757(93)90099-w
- Position paper: whole bowel irrigation. J Toxicol Clin Toxicol. 2004;42(6):843-54. doi: 10.1081/clt-200035932. Erratum in: J Toxicol Clin Toxicol. 2004;42(7):1000. Dosage error in article text. doi:10.1081/clt-200035932 PMID: 15533024.
- Iron. IBM Micromedex Solutions. Truven Health Analytics, Inc. Ann Arbor, MI. http://www.micromedexsolutions.com.
- Manoguerra, A. S., Erdman, A. R., Booze, L. L., Christianson, G., Wax, P. M., Scharman, E. J., Troutman, W. G. Iron Ingestion: an Evidence-Based Consensus Guideline for Out-of-Hospital Management. Clinical Toxicology, 2005; 43(6), 553–570. https://doi.org/10.1081/CLT-200068842







