Authors: Bricey Bayonnet, MD (EM Resident Physician, Atrium Health’s Carolinas Medical Center, Charlotte, NC); Christine Murphy, MD (EM Attending Physician; Medical Toxicologist, Atrium Health’s Carolinas Medical Center, Charlotte, NC) // Reviewed by: James Dazhe Cao, MD (@JamesCaoMD, Associate Professor of EM, Medical Toxicology, UT Southwestern Medical Center, Dallas, TX); Anthony Spadaro MD, (@TSpadaro91, Fellow in Medical Toxicology, Rutgers NJMS); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Case:
A 26-year-old male with a history of anxiety, major depressive disorder (MDD), post traumatic stress disorder (PTSD), and mood disorder presents to the emergency department (ED) via emergency medical services (EMS) after his roommate called after finding him on the floor of their apartment. His roommate found an empty pill bottle on the floor next to him. The bottle contained 100 mg quetiapine tablets, and 50 tablets were unaccounted for. On arrival, the patient is lethargic and has a Glasgow Coma Scale (GCS) score of 6. Vital signs on arrival are notable for a heart rate of 140, oxygen saturation of 90% on room air, and blood pressure of 90/40.
Questions:
- What are the symptoms of second-generation antipsychotic overdose?
- How is second-generation antipsychotic overdose diagnosed?
- What is the treatment for patients who have overdosed on second-generation antipsychotics?
Background:
- The first generation of antipsychotics (e.g., haloperidol, chlorpromazine) are known as typical antipsychotics and were developed in the 1950s.1
- Extrapyramidal symptoms (EPS) were common with the typical antipsychotics and resulted in the development of second-generation antipsychotics.1
- Atypical antipsychotics include both second- and third-generation antipsychotics.
- Second-generation antipsychotics (see Table 1 below) improve both positive and negative symptoms of schizophrenia and are less likely to be associated with EPS.1,2
- Most second-generation antipsychotics act as D2 antagonists and inhibit the 5-HT2A receptor.1
- Toxicity can result from overdose with predictable dose-dependent effects or can result from genetic or idiosyncratic differences that lead to toxicity in the setting of therapeutic dosing.1
- Third-generation antipsychotics include drugs like aripiprazole, brexpiprazole, and cariprazine.3
- These drugs are partial agonists at the D2 and 5-HT1A receptors with very high affinity for those receptors.
- These drugs also have active metabolites and very long half-lives with routine use and in the overdose setting.
- Atypical antipsychotics come in daily and long-acting forms.1
- Long-acting injectables (LAIs) have the lowest rate of self-harm attempts because they need to be injected by a healthcare professional.4
- The specific incidence of second-generation antipsychotic drug overdose is unknown, however, 4.7% of exposures reported to poison control centers in 2021 were related to antipsychotics or sedative-hypnotics with the majority of those exposures occurring in patients 20 years of age or older.5
- Second-generation antipsychotics (see Table 1 below) improve both positive and negative symptoms of schizophrenia and are less likely to be associated with EPS.1,2
Clinical Presentation:
- Second-generation antipsychotics are associated with several adverse effects that can occur in overdose or with therapeutic use.
- Atypical antipsychotics have lower incidence of EPS such as akathisia, dyskinesia, parkinsonism, or dystonia compared to typical antipsychotics, but these effects can still be observed with therapeutic use of these medications.
- In overdose, central nervous system (CNS) and cardiovascular complications are most common, however many organ systems can be affected.1,2,6
- Neurologic effects:
- Sedation is a primary concern with overdose.1,6
- Agitation, delirium, psychosis, and hallucinations can occur and may be incorrectly attributed to concurrent psychiatric illness.1
- Seizures may occur due to lowered seizure threshold.1,2
- Neuroleptic malignant syndrome (NMS) (hyperthermia, autonomic instability, rigidity, altered mental status [AMS]) can occur as well and is most often seen with clozapine but has been observed with other atypicals.2,7
- Cardiovascular effects:
- QRS prolongation can occur due to sodium channel blockade and is most often seen with quetiapine.2
- QTc prolongation occurs due to potassium rectifier channel blockade and is most prominent with ziprasidone.
- Rare instances of Torsade de Pointes may occur.1,6
- Hypotension and tachycardia may be observed secondary to á1-adrenergic blockade.2
- Antimuscarinic effects:
- Neurologic effects:
- May observe sedation, dry mouth, urinary retention, tachycardia, blurred vision, hyperthermia, flushed and dry skin, and delirium.1,2
- These effects are often associated with clozapine, olanzapine, and quetiapine.2
- Clozapine:
- In addition to the adverse effects mentioned above, there are specific monitoring guidelines and adverse effects that pertain to clozapine.
- Patients on clozapine are at risk for developing agranulocytosis and neutropenia and should have their neutrophil count monitored 8,9
- They are at additional risk for the development of myocarditis, QTc prolongation, and metabolic abnormalities including diabetes.8,9
- Pulmonary embolism has been observed in patients on clozapine.8
- GI hypomotility to the point of ileus has also been observed and is thought to be related to the anticholinergic properties of this medication.8
- Hypersalivation can occur.6
- Seizures have been observed and are dose-dependent.8
- Abrupt discontinuation of clozapine at doses as low as 50 mg/day has resulted in “cholinergic rebound” resulting in headache, nausea, vomiting and diarrhea.10
Table 1: Second-Generation Antipsychotics and Associated Adverse Effects
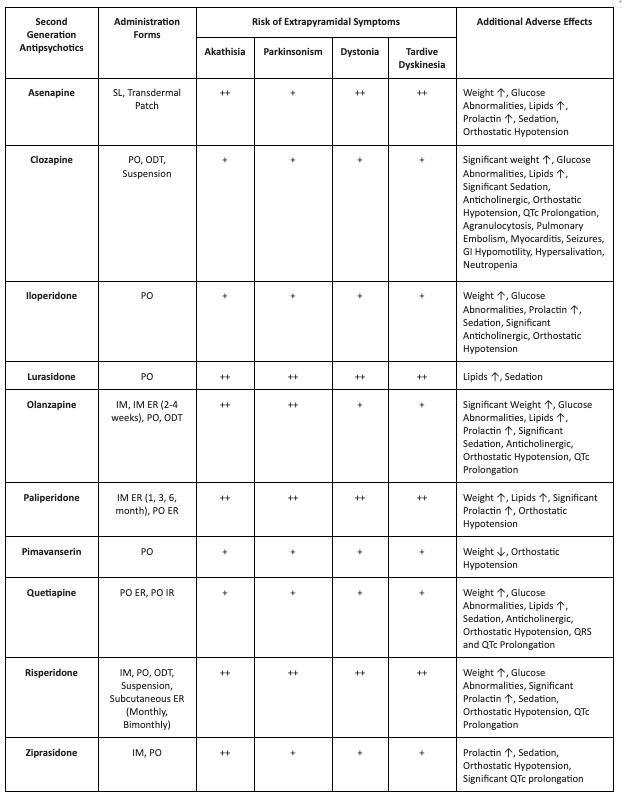
Adapted from: UpToDate8 with additional sources Micromedex9 and Riboldi, et al11
*SL=sublingual, IM=intramuscular, PO=oral, ODT=orally disintegrating tablets, ER=extended release, IR=immediate release. +to +++ = increasing risk of symptom
Diagnosis:
- Diagnosis will be predominantly based on clinical history and the patient’s exam findings.
- It is important to review home medications and over-the-counter medications present in the home to ensure no alternative explanations for observed symptoms are missed.
- When considering what laboratory studies or diagnostic tests to order take into account the variety of adverse effects that can occur with these medications and target testing to those you are concerned about.
- When there is concern for overdose, consider evaluation for additional co-ingestants such as acetaminophen or salicylate.
- The patient’s vital signs, including temperature, can be helpful in identifying effects related to these medications or guide the provider to look for signs of NMS when the patient has an elevated temperature.
- Recommend obtaining multiple EKGs to aid in the diagnosis of cardiotoxic effects such as dysrhythmias or interval widening, even if not apparent immediately after the overdose.
- A CBC can be helpful if the patient is on clozapine with concern for agranulocytosis.
- While non-specific and not diagnostic, consider obtaining a creatinine kinase concentration in patients where there is a concern for NMS or if they have had significant agitation and are at risk for developing rhabdomyolysis.
- Other laboratory studies that may be helpful in managing these patients include point-of-care glucose and electrolytes, including calcium and magnesium.
Management:
- Treatment is primarily supportive and aimed at the individual effects the patient is experiencing, whether an adverse effect of the drug with therapeutic use or in the setting of overdose.
Initial management strategies:
-
- In the setting of overdose, patients should have an IV established and be placed on the cardiac monitor.
- Monitor vital signs, including temperature and respiratory status closely.
- Consult a medical toxicologist or regional poison control (at 1-800-222-1222 in the United States).
Decontamination:
-
- Consider a dose of activated charcoal if they present within a few hours of ingestion and have normal mental status and active bowel sounds.1,2
Neurologic:
-
- In therapeutic second-generation antipsychotic use, patients may develop EPS. Therapy is targeted at symptomatic management.
- Akathisia, acute dystonic reactions, and tardive dyskinesia are often treated with a combination of diphenhydramine, benzodiazepines, and benztropine.12-14
- For patients with altered mental status, evaluate for and treat hypoglycemia.1
- Benzodiazepines are preferred as the first line of treatment for agitation or seizures.
- Consider barbiturates or propofol and an EEG if concerned for status epilepticus.
- Rigidity and hyperthermia should raise concerns for NMS.
- Initial management should be with benzodiazepines and rapid cooling efforts, which may necessitate sedation, intubation, and paralysis.1,2
- If there is no improvement, consider treatment with a dopamine agonist (bromocriptine) to reverse dopamine blockade or dantrolene.1,2
- In therapeutic second-generation antipsychotic use, patients may develop EPS. Therapy is targeted at symptomatic management.
Cardiovascular:
- Obtain an initial EKG to determine the patient’s baseline and repeat.
-
- If the EKG is normal in an asymptomatic patient at 6 hours, there is low likelihood of cardiac complication.1
-
-
- If the EKG is abnormal or patient continues with AMS at 6 hours, admit for cardiac monitoring for 24 hours.1
-
-
- If QTc is prolonged, replete potassium, magnesium and calcium abnormalities, consider frequent EKGs and monitor closely.2
-
-
- If Torsade de Pointes develops, defibrillate the patient if unstable, give magnesium, and consider overdrive pacing.2
-
-
- If the QRS is wide, > 120 msec, or the patient has ventricular dysrhythmia, a 1-2 mEq/kg IV bolus of sodium bicarbonate should be given in addition to continued investigation for possible co-ingestants.1,2
-
-
- Consider lidocaine if sodium bicarbonate fails.1
-
-
-
- Class IA (e.g., procainamide), IC (e.g., flecainide, propafenone), and class III (e.g., amiodarone) antidysrhythmics may worsen cardiac effects and should not be used.1
-
- Administer fluids for hypotension.
-
- If hypotension is refractory to IV fluids, initiate vasopressors. Consider agents with α1-adrenergic activity such as norepinephrine or phenylephrine.2
- Lipid emulsion has been considered due to the lipophilic nature of atypical antipsychotics; however, studies are limited on this topic, and this is an area that could benefit from further research.2,15,16
-
- Lipid emulsion is not suggested as a treatment for antipsychotic-related cardiac dysrhythmias.
Antimuscarinic effects:
-
-
- In therapeutic dosing, patients may experience antimuscarinic side effects including mydriasis, blurry vision, constipation due to slowed intestinal motility, and dry mouth.18
- Clozapine most commonly causes ileus; management of constipation includes adequate hydration and osmotic laxatives.18
- Additional information on antimuscarinic toxicity and treatment recommendations can be found here.
- In therapeutic dosing, patients may experience antimuscarinic side effects including mydriasis, blurry vision, constipation due to slowed intestinal motility, and dry mouth.18
-
Case Follow-up:
The patient was intubated for airway protection due to sedation. He received 2 L of lactated ringers IV for hypotension with improvement. His EKG demonstrated sinus tachycardia, with a QRS of 90 msec and QTc of 550 msec. Potassium and magnesium were replenished, and the QTc interval improved to 440 within two hours. The patient gradually improved. He was extubated on hospital day 2 and was able to be discharged to psychiatry on hospital day 5.
Clinical Pearls:
- Second-generation antipsychotic overdose is common, but the risk of life-threatening arrhythmia or serious CNS effects is rare.
- Common symptoms following overdose include sedation, tachycardia, and hypotension.
- Clozapine is unique when compared to other second-generation antipsychotics and requires additional monitoring.
- Differentiating clinical effects following an overdose of second-generation antipsychotics from adverse effects in therapeutic use can be difficult as many of the symptoms are the same.
- Management of atypical antipsychotic overdose is mainly supportive.
References:
- N. Juurlink D. Antipsychotics. In: Nelson LS, Howland MA, Lewin NA, Smith SW, Goldfrank LR, Hoffman RS, eds. Goldfrank’s Toxicologic Emergencies, 11e. New York, NY: McGraw-Hill Education; 2019. http://accesspharmacy.mhmedical.com/content.aspx?aid=1163014148.
- Minns AB, Clark RF. Toxicology and overdose of atypical antipsychotics. J Emerg Med. 2012;43(5):906-913.
- Citrome L. The ABC’s of dopamine receptor partial agonists – aripiprazole, brexpiprazole and cariprazine: the 15-min challenge to sort these agents out. Int J Clin Pract. 2015;69(11):1211-20.
- Pompili M. Adding suicide prevention to the triple advantages of injectable long-acting second-generation antipsychotics. Front Psychiatry. 2020;10.
- Gummin DD, Mowry JB, Beuhler M, et al. 2021 Annual Report of the National Poison Data System© (NPDS) from America’s Poison Centers: 39th Annual Report. Clinical Toxicol. 2022;60:12,1381-1643.
- Tan HH, Hoppe J, Heard K. A systematic review of cardiovascular effects after atypical antipsychotic medication overdose. Am J Emerg Med. 2009;27(5):607-616.
- Teo DCL, Wong HK, Tan SN. Atypical neuroleptic malignant syndrome precipitated by clozapine and quetiapine overdose: a diagnostic challenge. Innov Clin Neurosci. 2018;15(7-8):20-22.
- Jibson M. Second-generation antipsychotic medications: Pharmacology, administration, and side effects. UpToDate. https://www.uptodate.com/contents/second-generation-antipsychotic-medications-pharmacology-administration-and-side-effects. Published 2023. Accessed October 23, 2023.
- Micromedex. https://www.micromedexsolutions.com. Accessed October 23, 2023.
- Meyer JM, Stahl SM. The Clozapine Handbook: Stahl’s Handbooks. Cambridge: Cambridge University Press; 2019.
- Riboldi I, Cavaleri D, Capogrosso CA, et al. Practical guidance for the use of long-acting injectable antipsychotics in the treatment of schizophrenia. Psychol Res Behav Manag. 2022;15:3915-3929.
- Rice J. Akathisia. Core EM. https://coreem.net/core/akathisia. Published 2019. Accessed October 23, 2023.
- Nickson C. Stiff and Twisted. Life In The Fast Lane. https://litfl.com/acute-dystonic-reaction. Published 2020. Accessed October 23, 2023.
- Farkas J. Movement Disorder Emergencies. EmCrit. https://emcrit.org/ibcc/move/#acute_dystonia. Published 2022. Accessed October 23, 2023.
- Elgazzar FM, Elgohary MS, Basiouny SM, Lashin HI. Intravenous lipid emulsion as an adjuvant therapy of acute clozapine poisoning. Hum Exp Toxicol. 2021;40(7):1053-1063.
- Hubbard AM, House LM, Lee JM. Low-dose lipid emulsion for pediatric vasoplegic shock due to quetiapine and fluvoxamine overdose: a case report. J Emerg Crit Care Med Vol 6 (October 30, 2022) J Emerg Crit Care Med. 2022.
- Gosselin S, Hoegberg LC, Hoffman RS, Graudins A, Stork CM, Thomas SH, Stellpflug SJ, Hayes BD, Levine M, Morris M, Nesbitt-Miller A, Turgeon AF, Bailey B, Calello DP, Chuang R, Bania TC, Mégarbane B, Bhalla A, Lavergne V. Evidence-based recommendations on the use of intravenous lipid emulsion therapy in poisoning. Clin Toxicol (Phila). 2016 Dec;54(10):899-923.
- Stroup TS, Gray N. Management of common adverse effects of antipsychotic medications. World Psychiatry. 2018;17(3):341-356.







