Authors: Robert Nicholson, MD (EM Resident Physician, Carolinas Medical Center, Charlotte, NC) and Ann-Jeannette Geib, MD (EM Attending Physician, Medical Toxicologist, Carolinas Medical Center, Charlotte, NC) // Reviewed by: James Dazhe Cao, MD (@JamesCaoMD, Associate Professor of EM, Medical Toxicology, UT Southwestern Medical Center, Dallas, TX); Anthony Spadaro, MD (@TSpadaro91, Medical Toxicology Fellow, Rutgers New Jersey Medical School, Newark, NJ); Alex Koyfman, MD (@EMHighAK); Brit Long, MD (@long_brit)
Case:
45-year-old male is brought to the emergency department by his wife immediately after insufflating cocaine with complaints of muscle cramping. He denies any past medical history other than polysubstance abuse and depression. He is not currently prescribed any medicines and has no family medical history. Vital signs are as follows:
- Heart Rate 110 bpm
- Blood Pressure 175/100
- Oxygen Saturation 100% on room air
- Temperature 99.1 F
He is complaining of muscle spasms and pain. Exam is notable for tremulous extremities. Shortly after labs are obtained, he yells and arches his back. He becomes rigid in all extremities and his abdomen. There is no convulsive activity or eye deviation, and the patient is yelling in pain.
Questions:
- What is the differential diagnosis for toxicologic causes of severe muscle spasm and tetany?
- What are important clinical features differentiating strychnine and tetanus toxicity to aid with diagnosis?
- How does the clinical management of strychnine and tetanus differ?
STRYCHNINE
Background:
- Strychnine is an alkaloid, produced by the Strychnos nux-vomica plant1
- These plant seeds may be used in herbal remedies from Southeast Asia involving Ma Qian Zi or the slang nut and have also been processed into a colorless powder which has been found as a contaminant in cocaine and heroin2,3
- Strychnine may still be found in outdoor pesticides and rodenticides after being made illegal for use in indoor pesticides in 19892
- According to the 2022 Annual Report by the American’s Poison Centers, there were 85 documented exposures to strychnine between rodenticides and other sources with zero documented deaths4
- It has a fast absorption time and exerts effects in 15-30 minutes following oral ingestion5
- Strychnine acts by blocking the glycine receptor (Figure 1) on the post-synaptic neuron resulting in unopposed activation via glutamate from the excitatory axon terminal6
Figure 1. Site of action of strychnine and tetanus.

red X = target of strychnine
![]() = target of tetanus
= target of tetanus
Adapted from: Stephan J. Heterogeneous distribution and utilization of inhibitory neurotransmitter transporters. Neurotransmitter. 2015;2:10-14800/nt. 491. doi:10.14800/nt.491
Key Effects:
- Effects are usually seen within 15-30 minutes of exposure5
- Musculoskeletal system
-
- Initial tremor and myoclonus with progression to muscle spasm, risus sardonicus, and opisthotonos5
- Respiratory system
-
- Respiratory distress with progression to respiratory failure secondary to spasm of the respiratory musculature7
- Renal system
- Renal dysfunction secondary to rhabdomyolysis and acidosis8
Management:
- Early and aggressive airway management is important as patients can quickly progress from asymptomatic to severe respiratory distress5
- Benzodiazepines should be used to treat muscle spasms and decrease risk of rhabdomyolysis9
- If unable to control symptoms with benzodiazepines, patients may need paralysis while ventilated10
- Given the risk for hyperkalemia, a non-depolarizing agent should be used during rapid sequence intubation and for paralysis in the ventilated patient
- Activated charcoal may be considered to prevent absorption of ingested strychnine, however, may not be effective given its rapid absorption5
TETANUS
Background:
- Tetanus toxicity shares similar clinical features with strychnine intoxication but differs in its clinical history and pathophysiology. It is still a vaccine-preventable disease.
- Tetanus is a potentially fatal condition with a case-fatality rate as high as 43% in resource-poor countries11
- The case-fatality rate is also lower in resource-rich countries, and only 297 cases were reported in the United States between 2009 and 201812
- The tetanus toxin, tetanospasmin, is an exotoxin produced by the anaerobic bacillus Clostridium tetani which is found in the soil and inoculates wounds with an incubation period from 3-21 days, with an average of 8 days
- Once a wound is inoculated, the toxin travels through retrograde axonal transport to the spinal cord where it prevents exocytosis of glycine and GABA from the presynaptic inhibitory neuron (Figure 1) resulting in unopposed activity from the excitatory axon terminal13,14
Clinical Classifications of tetanus:12
- Generalized tetanus – whole-body involvement usually evolving in a descending pattern
- Neonatal tetanus – affecting neonates, most commonly secondary to unvaccinated mothers or infection of the umbilical stump
- Localized tetanus – affects the local area surrounding the wound
- Cephalic tetanus – localized form of tetanus affecting the facial nerves most commonly from a local wound
Key Effects:
- Illness duration for tetanus may last 4-6 weeks
- Musculoskeletal system
-
- Trismus is the most common presenting symptom found in up to 75% of patients15
-
- “Spatula test” during stimulation of the posterior pharyngeal wall is positive if it produces masseter spasm rather than the usual gag reflex16
-
- Other musculoskeletal effects include generalized muscle spasm, opisthotonos, rhabdomyolysis, and risus sardonicus
-
- Given the severity of tonic muscular contractions, muscle and tendon injuries, joint dislocations, and long bone fractures are possible17,18
- Respiratory system
-
- Respiratory distress and failure are secondary to respiratory muscle spasm
-
- Vocal cord and laryngospasm in severe illness19
- Renal system
-
- Potential renal failure secondary to rhabdomyolysis20
- Nervous system
- Autonomic hyperactivity with subsequent hypertension and increased risk for dysrhythmias21
Management:
- Benzodiazepines should be used for control of muscle spasms and in severe cases, a non-depolarizing paralytic
- Minimize patient stimulation – place patient in dark quiet room
- Wound irrigation and debridement are critical for preventing additional toxin in the local tissues from undergoing retrograde axonal transport
- Antibiotic therapy to eliminate C. tetani infection is also indicated.
-
- First line therapy: metronidazole 500mg IV every 6-8 hours
-
- Second line therapy: penicillin G 2 to 4 million units IV every 4-6 hours
-
- Metronidazole has decreased mortality compared with penicillin and may be associated with decreased spasm, since penicillin in high doses is associated with CNS excitability21-23
- Patients should also be administered tetanus immune globulin with 500U administered via the IM or IV route with similar efficacy to the previously used higher doses
- Magnesium sulfate has been studied in multiple trials to decrease severity of muscle spasms when compared to benzodiazepines and may have a beneficial effect on symptoms of autonomic hyperactivity24-26
-
- Loading dose of 75 to 80 mg/kg in 30 minutes followed by an infusion rate of 2 g/hour for patients <60 years of age and 1 g/hour for patients >60 years
- Intrathecal baclofen use has been reported in case reports and series with doses ranging from 500 to 2,000 μg daily. A decrease in spasticity is reported, but formal trial and/or comparative data are lacking. Several cases of intrathecal catheter infection have been reported, and use of baclofen requires intensive monitoring and likely mechanical ventilation27
- In patients requiring endotracheal intubation, tracheostomy should be considered after approximately 10 days on the ventilator given risk for vocal cord injury and tracheal stenosis with prolonged orotracheal intubation
- If rapid sequence intubation is required, a non-depolarizing agent should be used.
- After recovery from illness, repeat vaccination with the tetanus series will be required as infection does not confer immunity
Clinical Pearls:
Strychnine
- Alkaloid found in rodenticides and herbal remedies which may be a contaminant of recreational drugs
- Exerts its effect by blocking receptors for inhibitory neurotransmitters resulting in overactive muscle stimulation from excitatory neurons
- Rapid onset of symptoms from time of ingestion
- Muscle spasm may be severe enough to cause respiratory distress and cardiac arrest
- Supportive care with benzodiazepines for treatment of muscle spasm
Tetanus
- Caused by the exotoxin produced from Clostridium tetani with an incubation period ranging from 3-21 days
- Prevents exocytosis of inhibitory neurotransmitters into the post-synaptic cleft resulting in excessive activity from the excitatory neuron and subsequent muscle spasm
- Exerts its main effects on the musculoskeletal, respiratory, and nervous systems through sustained muscle spasm, respiratory failure, and autonomic hyperactivity
- Management includes wound care, antibiotics, immune globulin, benzodiazepines, airway management, and potentially magnesium sulfate and intrathecal baclofen
- Illness duration may be prolonged
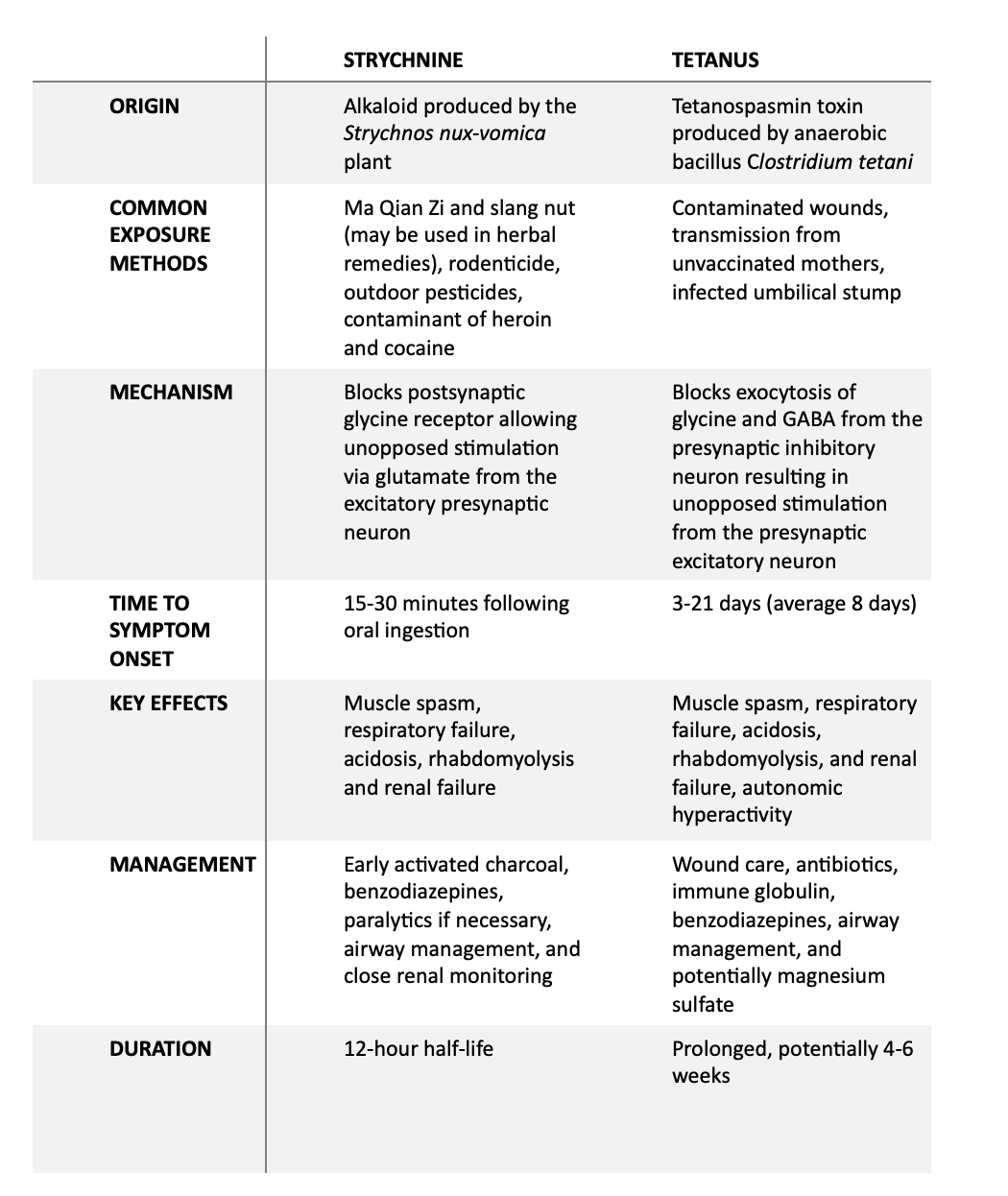
Table 1: Comparison of strychnine and tetanus
References:
- Duverneuil C, de la Grandmaison GL, de Mazancourt P, Alvarez JC. Liquid chromatography/photodiode array detection for determination of strychnine in blood: a fatal case report. Forensic Sci Int. 2004;141(1):17-21. doi:10.1016/j.forsciint.2003.12.010
- Otter J, D’Orazio JL. Strychnine Toxicity. In: StatPearls. StatPearls Publishing; 2022. Accessed April 27, 2022. http://www.ncbi.nlm.nih.gov/books/NBK459306/
- O’Callaghan WG, Joyce N, Counihan HE, Ward M, Lavelle P, O’Brien E. Unusual strychnine poisoning and its treatment: report of eight cases. Br Med J Clin Res Ed. 1982;285(6340):478-478. doi:10.1136/bmj.285.6340.478
- Gummin DD, Mowry JB, Beuhler MC, et al. 2022 Annual Report of the National Poison Data System®(NPDS) from America’s Poison Centers®: 40th Annual Report. Clin Toxicol (Phila). 2023;61(10):717-939. doi:10.1080/15563650.2023.2268981
- Wood DM, Webster E, Martinez D, Dargan PI, Jones AL. Case report: Survival after deliberate strychnine self-poisoning, with toxicokinetic data. Crit Care. 2002;6(5):456. doi:10.1186/cc1549
- Probst A, Cortés R, Palacios JM. The distribution of glycine receptors in the human brain. A light microscopic autoradiographic study using [3H]strychnine. Neuroscience. 1986;17(1):11-35. doi:10.1016/0306-4522(86)90222-8
- Teitelbaum DT, Ott JE. Acute strychnine intoxication. Clin Toxicol. 1970;3(2):267-273. doi:10.3109/15563657008990475
- Boyd RE, Brennan PT, Deng JF, Rochester DF, Spyker DA. Strychnine poisoning. Recovery from profound lactic acidosis, hyperthermia, and rhabdomyolysis. Am J Med. 1983;74(3):507-512. doi:10.1016/0002-9343(83)90999-3
- Hardin J, Griggs R. DIAZEPAM TREATMENT IN A CASE OF STRYCHNINE POISONING. The Lancet. 1971;298(7720):372-373. doi:10.1016/S0140-6736(71)90085-7
- Smith BA. Strychnine poisoning. J Emerg Med. 1990;8(3):321-325. doi:10.1016/0736-4679(90)90013-l
- Woldeamanuel YW, Andemeskel AT, Kyei K, Woldeamanuel MW, Woldeamanuel W. Case fatality of adult tetanus in Africa: Systematic review and meta-analysis. J Neurol Sci. 2016;368:292-299. doi:10.1016/j.jns.2016.07.025
- Pinkbook: Tetanus | CDC. Published August 17, 2021. Accessed April 27, 2022. https://www.cdc.gov/vaccines/pubs/pinkbook/tetanus.html
- Lalli G, Bohnert S, Deinhardt K, Verastegui C, Schiavo G. The journey of tetanus and botulinum neurotoxins in neurons. Trends Microbiol. 2003;11(9):431-437. doi:10.1016/s0966-842x(03)00210-5
- Schiavo G, Benfenati F, Poulain B, et al. Tetanus and botulinum-B neurotoxins block neurotransmitter release by proteolytic cleavage of synaptobrevin. Nature. 1992;359(6398):832-835. doi:10.1038/359832a0
- Giannini L, Maccari A, Chiesa V, Canevini MP. Trismus, the first symptom in a challenging diagnosis of Tetanus. BMJ Case Rep. 2016;2016:bcr2015213897. doi:10.1136/bcr-2015-213897
- Paterson AW, Ryan W, Rao-Mudigonda VV. Trismus: or is it tetanus? A report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(4):437-441. doi:10.1016/j.tripleo.2005.04.013
- Alfery DD, Rauscher LA. Tetanus: a review. Crit Care Med. 1979;7(4):176-181. doi:10.1097/00003246-197904000-00007
- Thachil RT, Philip B, Sridhar CB. Temporomandibular dislocation: a complication of tetanus. J Trop Med Hyg. 1993;96(1):60-61.
- Bunch TJ, Thalji MK, Pellikka PA, Aksamit TR. Respiratory failure in tetanus: case report and review of a 25-year experience. Chest. 2002;122(4):1488-1492. doi:10.1378/chest.122.4.1488
- Li L, Liu Z. Rhabdomyolysis with acute anuria renal failure caused by surgical injection-induced tetanus in an adult. Clin Med. 2021;21(1):e103-e105. doi:10.7861/clinmed.2020-0841
- Lin TS, Chen LK, Lin TY, Wen SH, Chen MC, Jan RH. Autonomic Dysfunction Because of Severe Tetanus in an Unvaccinated Child. Pediatr Neonatol. 2011;52(3):169-171. doi:10.1016/j.pedneo.2011.03.010
- Afshar M, Raju M, Ansell D, Bleck TP. Narrative review: tetanus-a health threat after natural disasters in developing countries. Ann Intern Med. 2011;154(5):329-335. doi:10.7326/0003-4819-154-5-201103010-00007
- Ahmadsyah I, Salim A. Treatment of tetanus: an open study to compare the efficacy of procaine penicillin and metronidazole. Br Med J Clin Res Ed. 1985;291(6496):648-650.
- Farrar J, Yen L, Cook T, et al. Tetanus. J Neurol Neurosurg Psychiatry. 2000;69(3):292-301. doi:10.1136/jnnp.69.3.292
- Ogun S, Ogunniyi A. Comparison of the efficacy of magnessium sulphate and diazepam in the control of tetanus spasms. Sci Res Essays. 2008;3.
- Thwaites CL, Yen LM, Cordon SM, et al. Effect of magnesium sulphate on urinary catecholamine excretion in severe tetanus. Anaesthesia. 2008;63(7):719-725. doi:10.1111/j.1365-2044.2008.05476.x
- Rodrigo C, Fernando D, Rajapakse S. Pharmacological management of tetanus: an evidence-based review. Crit Care. 2014;18(2):217. doi:10.1186/cc13797
- Ali G, Kamal M, Khan AN. COMPARISON OF THE EFFICACY OF MAGNESIUM SULPHATE AND DIAZEPAM IN THE CONTROL OF TETANUS SPASM. J Postgrad Med Inst. 2011;25(2). Accessed April 27, 2022. https://jpmi.org.pk/index.php/jpmi/article/view/95








