Originally posted on Trauma ICU Rounds on April 24, 2020. Follow Trauma ICU Rounds (@traumaicurounds) and Dr. Kim (@dennisyongkim) to learn more on simplifying trauma critical care together.
Summary
Before the COVID19 pandemic hit the US and California became the first state to issues Stay Safe at Home orders, I had an opportunity to meet with Dr. Matt Martin from Scripps Mercy Hospital in San Diego at the 91st Annual Pacific Coast Surgical Association (PCSA) Meeting in Carlsbad, CA (Feb. 14-17, 2020) for our first interview on Rounds.
During the course of our discussion we reviewed several recent changes in our resuscitation strategy of injured patients. We also discussed endpoints of resuscitation and emphasized the need to first, understand the clinical problem in need of resuscitation and, second, identify the targets or goals of resuscitation.
Learning Objectives
By the end of Rounds, you should have an appreciation of:
-
The initial assessment of critically ill and injured patients.
-
Methods for identifying the presence or absence of shock
-
Various modalities for identifying patients in need of resuscitation
Take Home Points
-
Always start your assessment by asking yourself, “What’s going to kill my patient immediately?” This question is followed by, “What common problems or clinical diagnoses should I rule out?”. Only then should you start thinking about zebras.
-
Whole blood is the best individual fluid you can give. Consider a plasma first resuscitation strategy in bleeding trauma patients.
-
Every time you assess a patient, classify them as being either “sick” of “not sick”.
-
Resuscitation endpoints should be tailored on the basis of what condition is in need of resuscitation AND identifying not just our endpoints but where are we in terms of start points.
Time Stamps
-
00:13 Introduction
-
01:39 Military Experience – Pre-hospital & In-hospital Assessment
-
04:03 Resuscitation Fluids & Whole Blood
-
06:08 Endpoints in Patients with Suspected TBI
-
07:28 Shock Index, Narrowed Pulse Pressure
-
09:42 Whole Blood Resuscitation
-
11:44 Pre-hospital biomarkers (POC lactate)
-
13:45 StO2 Monitoring
-
14:53 Permissive Hypotension following Penetrating Torso Trauma
-
16:50 Popping the Clot
-
18:11 Matt Martin’s Approach to the “Sick” vs. “Not Sick” Trauma Patient
-
23:05 ACS Classification of Hemorrhage
-
24:06 Utility of Urine Output Monitoring in “Sick” Patients
-
25:47 Utility of Lactate & Base Deficit
-
27:49 Lactate Clearance & Touching on Type A vs. Type B Lactic Acidosis
-
29:28 Over-Resuscitation & the “Lactobolus Reflex”
-
31:31 A Normal Lactate Means Nothing in Mesenteric Ischemia
-
34:06 Application of Ultrasound during Active Resuscitation of Critically Ill Patients
-
39:54 CVP Sucks
-
40:34 Final Messages
-
42:30 Outro
Potential Indicators of the Need for Transfusion or Emergent Hemorrhage Control Intervention
Shock Index (SI) = HR / SBP (HIGH SI defined as >0.8)
Narrow Pulse Pressure (PP) <=30 mmHg (varies with age)
Assessment of Blood Consumption (ABC) Score
-
Penetrating mechanism
-
Arrival systolic BP 90 mmHg or less
-
Arrival heart rate > 120 bpm
-
+ FAST
*score <2, unlikely to require massive transfusion; sensitivity (75 – 90%) & specificity (67 – 88%)
ACS Classification of Hemorrhagic Shock
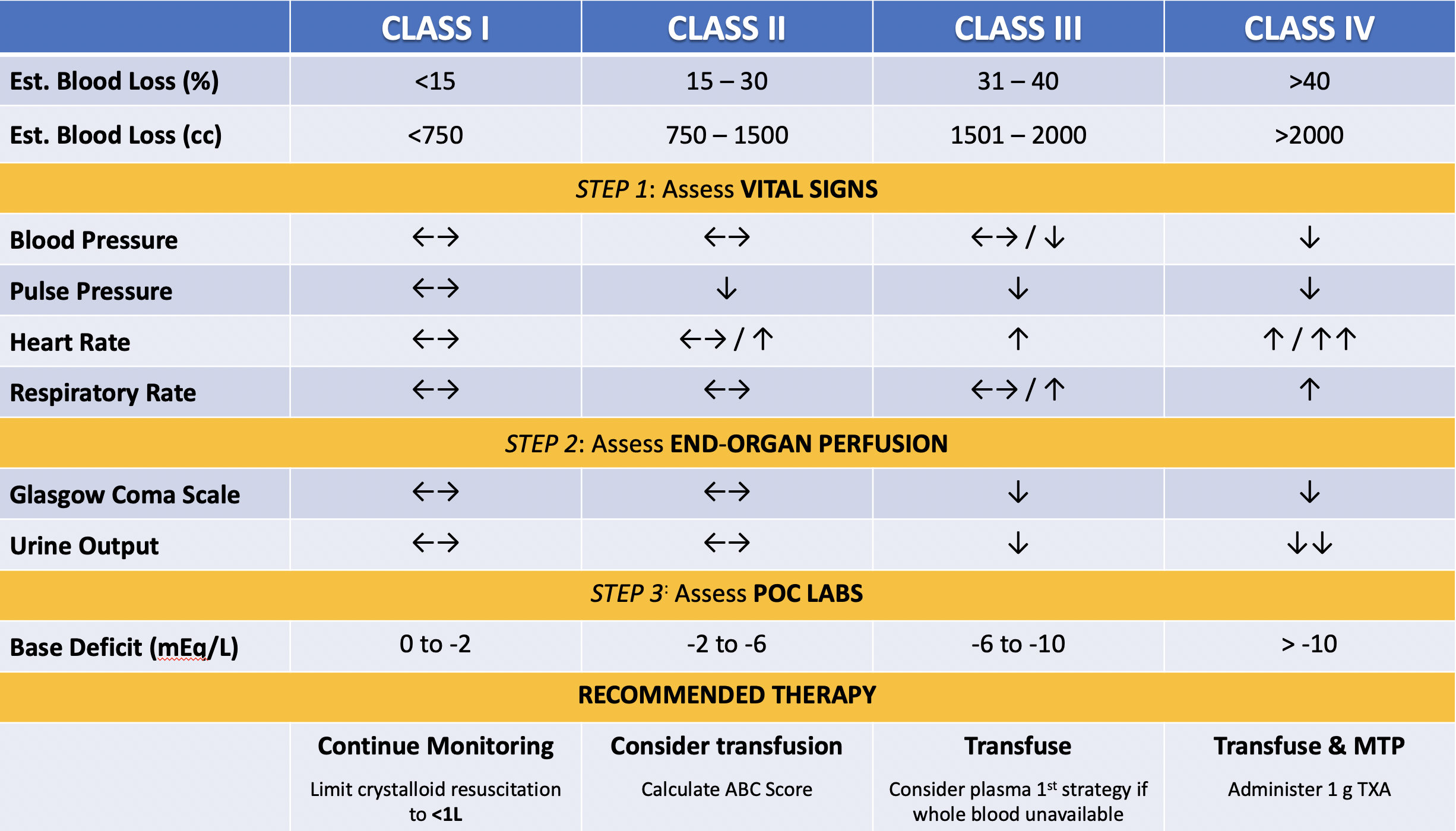
Regarding the classification of hemorrhage shock, always start with the patient’s vitals. The finding of a narrow pulse pressure should alert you to the potential for bleeding. For example, if a patient arrives following a GSW to the abdomen and the initial BP reads 140/115, this should not be interpreted as normal!!!! In hemorrhagic shock, the loss of intravascular volume results in decreased preload, stroke volume, and cardiac output.
Remember the mean arterial pressure (MAP) is the product of cardiac output (Q) & systemic vascular resistance (SVR). If cardiac output is decreased due to a decreased stroke volume, the body will attempt to compensate by increasing vascular tone. This may manifest as an elevated diastolic pressure or a narrow pulse pressure. Check out a study we published on this topic listed in the Recommended Reading below.
Mental status or GCS is a readily accessible and quick measure of the presence or absence of hypoxic encephalopathy. Although many confounders may alter the exam (TBI, alcohol, drugs, etc.) an altered mental status should always alert you tot he presence of brain hypoxia. In the setting of trauma the number 1-2-and3 causes of shock are BLEEDING-BLEEDING-BLEEDING!!!
For patients recognized as being in shock, immediate intervention is required followed by REASSESSMENT & REEVALUATION. Every intervention should be immediately followed by asking if patients have a desired response. Patients typically respond in 1 of 3 ways. They may RESPOND. They may TRANSIENTLY RESPOND or they may NOT RESPOND. In the latter 2 cases, you should have a very low threshold for transfusing blood & blood products NOT salt water!!!!
Recommended Readings
TCCC Guidelines for Medical Personnel 1 August 2019
https://www.naemt.org/education/naemt-tccc
https://www.naemt.org/docs/default-source/education-documents/tccc/tccc-mp-updates-190801/tccc-guidelines-for-medical-personnel-190801.pdf?sfvrsn=cc99d692_2
Hypertonic Saline
Bulger EM, May S, Brasel KJ, Schreiber M, Kerby JD, Tisherman SA, Newgard C, Slutsky A, Coimbra R, Emerson S, Minei JP, Bardarson B, Kudenchuk P, Baker A, Christenson J, Idris A, Davis D, Fabian TC, Aufderheide TP, Callaway C, Williams C, Banek J, Vaillancourt C, van Heest R, Sopko G, Hata JS, Hoyt DB; ROC Investigators. Out-of-hospital hypertonic resuscitation following severe traumatic brain injury: a randomized controlled trial. JAMA. 2010 Oct 6;304(13):1455-64.
Bulger EM, May S, Kerby JD, Emerson S, Stiell IG, Schreiber MA, Brasel KJ, Tisherman SA, Coimbra R, Rizoli S, Minei JP, Hata JS, Sopko G, Evans DC, Hoyt DB; ROC investigators. Out-of-hospital hypertonic resuscitation after traumatic hypovolemic shock: a randomized, placebo controlled trial. Ann Surg. 2011 Mar;253(3):431-41.
Whole Blood & Plasma
Walsh M, Fries D, Moore E, Moore H, Thomas S, Kwaan HC, Marsee MK, Grisoli A, McCauley R, Vande Lune S, Chitta S, Vyakaranam S, Waxman D, McCurdy MT, Zimmer D, Patel B, Thachil J. Whole Blood for Civilian Urban Trauma Resuscitation: Historical, Present, and Future Considerations. Semin Thromb Hemost. 2020 Mar;46(2):221-234.
Reitz KM, Moore HB, Guyette FX, Sauaia A, Pusateri AE, Moore EE, Hassoune A, Chapman MP, Daley BJ, Miller RS, Harbrecht BG, Claridge JA, Phelan HA, Brown JB, Zuckerbraun BS, Neal MD, Yazer MH, Sperry JL. Prehospital plasma in injured patients is associated with survival principally in blunt injury: Results from two randomized prehospital plasma trials. J Trauma Acute Care Surg. 2020 Jan;88(1):33-41.
Sperry JL, Guyette FX, Brown JB, Yazer MH, Triulzi DJ, Early-Young BJ, Adams PW, Daley BJ, Miller RS, Harbrecht BG, Claridge JA, Phelan HA, Witham WR, Putnam AT, Duane TM, Alarcon LH, Callaway CW, Zuckerbraun BS, Neal MD, Rosengart MR, Forsythe RM, Billiar TR, Yealy DM, Peitzman AB, Zenati MS; PAMPer Study Group. Prehospital Plasma during Air Medical Transport in Trauma Patients at Risk for Hemorrhagic Shock. N Engl J Med. 2018 Jul 26;379(4):315-326.
Moore HB, Moore EE, Chapman MP, McVaney K, Bryskiewicz G, Blechar R, Chin T, Burlew CC, Pieracci F, West FB, Fleming CD, Ghasabyan A, Chandler J, Silliman CC, Banerjee A, Sauaia A. Plasma-first resuscitation to treat haemorrhagic shock during emergency ground transportation in an urban area: a randomised trial. Lancet. 2018 Jul 28;392(10144):283-291
Shock Index, Narrow Pulse Pressure, ABC Score & Compensatory Reserve Index
Priestley EM, Inaba K, Byerly S, Biswas S, Wong MD, Lam L, Benjamin E, Demetriades D. Pulse Pressure as an Early Warning of Hemorrhage in Trauma Patients. J Am Coll Surg. 2019 Aug;229(2):184-191.
Warren J, Moazzez A, Chong V, Putnam B, Neville A, Singer G, Deane M, Kim DY. Narrowed pulse pressure predicts massive transfusion and emergent operative intervention following penetrating trauma. Am J Surg. 2019 Dec;218(6):1185-1188.
Kimura A, Tanaka N. Reverse shock index multiplied by Glasgow Coma Scale score (rSIG) is a simple measure with high discriminant ability for mortality risk in trauma patients: an analysis of the Japan Trauma Data Bank. Crit Care. 2018 Apr 11;22(1):87.
Nunez TC, Voskresensky IV, Dossett LA, Shinall R, Dutton WD, Cotton BA. Early prediction of massive transfusion in trauma: simple as ABC (assessment of blood consumption)? J Trauma. 2009 Feb;66(2):346-52.
Johnson MC, Alarhayem A, Convertino V, Carter R 3rd, Chung K, Stewart R, Myers J, Dent D, Liao L, Cestero R, Nicholson S, Muir M, Schwacha M, Wampler D, DeRosa M, Eastridge B. Compensatory Reserve Index: Performance of A Novel Monitoring Technology to Identify the Bleeding Trauma Patient. Shock. 2018 Mar;49(3):295-300.
Liu NT, Holcomb JB, Wade CE, Salinas J. Improving the prediction of mortality and the need for life-saving interventions in trauma patients using standard vital signs with heart-rate variability and complexity. Shock. 2015 Jun;43(6):549-55.
Permissive Hypotension
Bickell WH, Wall MJ Jr, Pepe PE, Martin RR, Ginger VF, Allen MK, Mattox KL. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med. 1994 Oct 27;331(17):1105-9.
Hirshberg A, Hoyt DB, Mattox KL. From “leaky buckets” to vascular injuries: understanding models of uncontrolled hemorrhage. J Am Coll Surg. 2007 Apr;204(4):665-72.
Lactate & Base Deficit
Davis JW, Shackford SR, Mackersie RC, Hoyt DB. Base deficit as a guide to volume resuscitation. J Trauma. 1988 Oct;28(10):1464-7.
Davis JW, Dirks RC, Kaups KL, Tran P. Base deficit is superior to lactate in trauma. Am J Surg. 2018 Apr;215(4):682-685.
Husain FA, Martin MJ, Mullenix PS, Steele SR, Elliott DC. Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg. 2003 May;185(5):485-91.
Martin MJ, FitzSullivan E, Salim A, Berne TV, Towfigh S. Use of serum bicarbonate measurement in place of arterial base deficit in the surgical intensive care unit. Arch Surg. 2005 Aug;140(8):745-51.
Ultrasound
Ferrada P. Image-based resuscitation of the hypotensive patient with cardiac ultrasound: An evidence-based review. J Trauma Acute Care Surg. 2016 Mar;80(3):511-8
Nowack T, Christie DB 3rd. Ultrasound in trauma resuscitation and critical care with hemodynamic transesophageal echocardiography guidance. J Trauma Acute Care Surg. 2019 Jul;87(1):234-239.
Central Venous Pressure & Arterial Pressure Waveform Analysis
Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest. 2008 Jul;134(1):172-8.
Plurad DS, Chiu W, Raja AS, Galvagno SM, Khan U, Kim DY, Tisherman SA, Ward J, Hamill ME, Bennett V, Williams B, Robinson B. Monitoring modalities and assessment of fluid status: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2018 Jan;84(1):37-49







