Originally published on Ultrasound G.E.L. on 9/26/26 – Visit HERE to listen to accompanying PODCAST! Reposted with permission.
Follow Dr. Michael Prats, MD (@PratsEM), Dr. Creagh Bougler, MD (@CreaghB), and Dr. Jacob Avila, MD (@UltrasoundMD) from Ultrasound G.E.L. team!
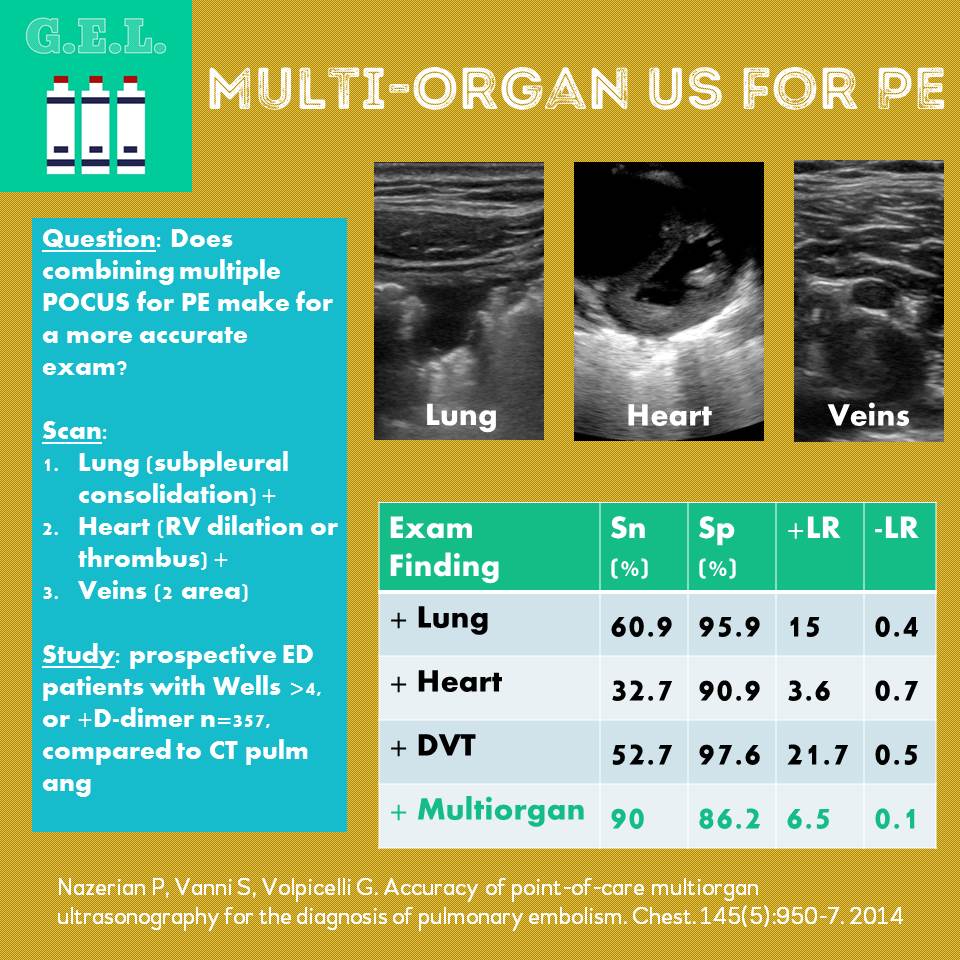
Accuracy of Point-of-Care Multiorgan Ultrasonography for the Diagnosis of Pulmonary Embolism
Review article that references this article
Background
PE is a common consideration in patients with chest pain, dyspnea, or cardiac arrest. We have had increase in CT use for PE disproportionate to increase in PE. Ultrasound has advantages over CT such as no radiation, use in unstable patients, no contrast needed that can damage kidneys. Prior studies have shown that ultrasound findings of right heart strain, subpleural infarcts, and DVT can be used to help diagnose PE; however, each alone is not sensitive enough to rule out PE. This study aims to see if combining these tests into a single “multi-organ” scan would have a better sensitivity for PE.
Questions
How accurate is an ultrasound of the heart, lungs, and veins in diagnosing PE compared to CT?
Can ultrasound be used to create a diagnostic algorithm that would reduce CT and not lead to missed PE?
Population
Multi-center, 3 Italian Hospitals (2 university, 1 community)
Inclusion: >18 yo + suspected of having PE
Who did the ultrasounds?
13 investigators
-1 emergency physician with expertise
-8 EP with 5 years of POCUS experience
-4 residents with “focus in cardiac, vein, and lung ultrasound” (2 EM, 2 IM)
Design
Consecutive patients, suspected of having PE
All got Wells score and D-dimer
If Wells <5 and D-dimer <500 ng/mL → no more testing
If Wells >4 or D-dimer ≥500 ng/mL → CT pulmonary angiography. Ultrasound performed prior to and within 3 hours of CT
If Ultrasound negative for PE, investigator asked to specify alternative diagnosis based on US
CTs read by 2 radiologists “expert in PE diagnosis” blinded to clinical data and ultrasound
Power analysis: maximum sensitivity of scans previously reported to be 80%. Set type 1 error at 5% → if sample size 330 then 90% power to detect 10% absolute difference between US and CT
Intervention
All patients got Wells score and D-dimer. If not determined to be “low risk” –> received CT and 3 part US
Scan
Lung – 4-8 MHz linear probe or 3.5-5 MHz curved array probe. Long and oblique scans on anterior and posterior chest in supine position. Lateral decubitus or sitting for dorsal areas. Looking for subpleural infarcts. Also noted consolidations, effusions, interstitial syndrome.
5 min sono post on subpleural consolidation in PE
Heart – 2-5 MHz phased array probe. RV dilation with one of the following: a) right to left ventricular end diastolic diameter >0.9 in apical 4 chamber of subcostal b) RV end diastolic diameter >30 mm in parasternal view c)Thrombus in right side of heart. Effusion and dissections were noted also.
Vein – 4-8 MHz linear probe. Short axis of common and superficial femoral veins, popliteal veins. DVT = absence of total vein collapse during compression.
Considered positive scan if any of the three was positive.
Results
510 patients enrolled, 97 (19%) were ruled out with d-dimer and Wells score 56 excluded – pregnancy (3), did not consent(4), CT contraindicated (23), CT inconclusive (6), or US not performed(20) So N = 357
110 had PE on CT (30.8%), K between radiologists K = 0.95 PE presents in 41.1% of Wells > 4 (3 had negative D-dimer) If Wells ≤ 4 and positive D-dimer – 21% had PE
Main Results
Multiorgan US – Sensitivity 90% (82.8-94.9), Specificity 86.2% (81.3-90.3), +LR 6.5, -LR 0.12
MO US + Alternate – Sens 100% (96.7-100), Spec 42.9% (36.7-49.3%), +LR 1.75, -LR 0
Lung alone 60.0% sens, 95.9% spec, +LR 15, -LR 0.4
Heart alone 32.7% sens, 90.9% spec, + LR 3.6, -LR 0.7
Vein alone 52.7% sens, 97.6% spec, +LR 21.7, -LR 0.5
Other Interesting Findings
133 patients had positive US, 99 had PE (74.4%)
PE was in 11 of 224 patients (4.9%) with negative US
Negative US + negative d-dimer → none had PE (n = 55)
106 patients with US negative for PE (47.3%) had alternate diagnoses (pneumonia, diffuse interstitial syndrome, pleural effusion, pericardial effusion, aortic dissection) → none had PE on CT
64.9% of + lung findings were posterior bases
Algorithm was developed based on this data. Says you don’t need to do CT if you have a DVT or if you do US and find an alternate cause for symptoms – would have avoided CT in 50% of study population
Limitations
US performed by skilled providers
Excluded 20 where US was not performed – unclear why, but that may make it less “feasible”
Don’t know how long it took
CT pulmonary angiography may not be best gold standard since it can provide both false negatives and false positives (especially with regard to possible “sub-clinical” PEs)
Take Home Points
1. Multiorgan Lung ultrasound is feasible and better than single organ scans to rule out PE. 90% sensitive, -LR of 0.12.
2. Multiorgan US negative for PE + finds an alternate diagnosis → PE very unlikely
Our score