Originally published on Ultrasound G.E.L. on 4/9/18 – Visit HERE to listen to accompanying PODCAST! Reposted with permission.
Follow Dr. Michael Prats, MD (@PratsEM), Dr. Creagh Bougler, MD (@CreaghB), and Dr. Jacob Avila, MD (@UltrasoundMD) from Ultrasound G.E.L. team!
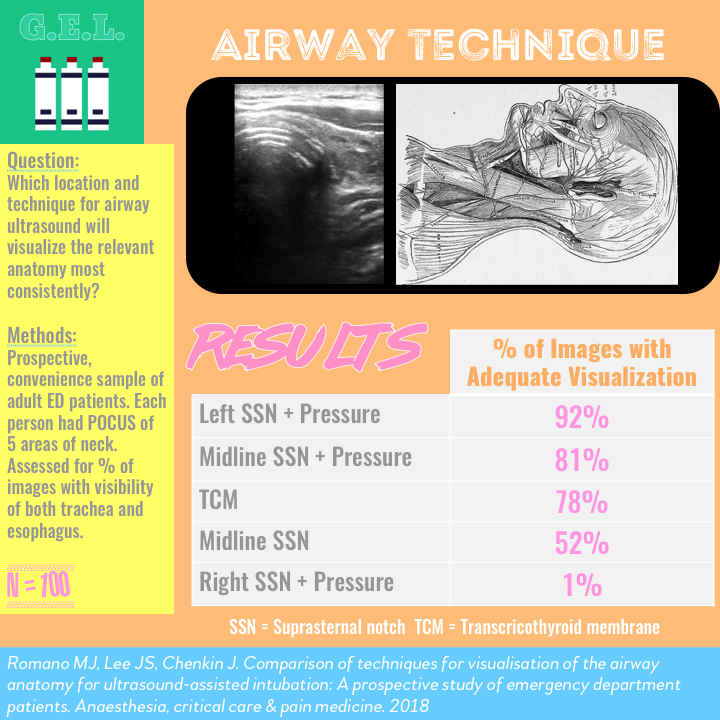
Comparison of techniques for visualisation of the airway anatomy for ultrasound-assisted intubation: A prospective study of emergency department patients
Anaesth Crit Care Pain Med Feb 2018 – Pubmed Link
Take Home Points
1. The best technique to visualize the tracheal and esophagus simultaneously is with the transducer to the left of the suprasternal notch using light pressure.
2. We don’t know if this holds true in patients who are actually getting intubated.
Background
Intubating the esophagus can be useful in some instances…but not when the patient requires a definitive airway. Accidental intubation of the esophagus happens every so often during attempted tracheal intubation (5-8% per a study these authors site), but the real trouble is when it is not recognized. There are many ways to confirm the intubation including auscultation, capnography, and xray. Apparently qualitative capnography has a 7% false negative rate and 3% false positive rate. US has been offerred up as a quick option to confirm ETT at bedside. As a bonus, it can also tell if the ET tube is in a main stem bronchus. Plus – you get to determine success in real time, not only after bagging the patient. We have covered tracheal ultrasound for intubation on a prior episode, and it seems to be fairly accurate. The next question, explored by these authors, is what is the best technique to obtain this non-standardized view?
Questions
Which anatomic location for airway ultrasound will visualize the relevant anatomy most frequently?
Does moving the transducer off midline help?
Does adding pressure help?
Population
Convenience sample, stable, nonintubated patients. Authors from Canada.
Inclusion:
- In Emergency Department (ED)
- Adults > 18 yo
- Presented to the ED when investigators were available
Exclusion:
- Intubated
- Those who could not tolerate supine
- Unstable, life-threatening injuries requiring immediate intervention
Design
Prospective observational
Urban teaching hospital
Exams were performed on ED patients
Images were reviewed and assessed for presence of both trachea and esophagus. Considered “adequate” if these were at last partially visible.
Power calculation: 96 patients needed
Intervention
Each patient placed supine, flexed neck, extended head. They then underwent 7 different views – combinations of different placement of transducer, laterality, and with and without pressure.
Transcricothyroid method (TCM) (#1)
Suprasternal notch method (SSN) midline (#2)
SSN + pressure (#3)
SSN to left (#4)
SSN to left + pressure (#5)
SSN to right (#6)
SSN to right + pressure (#7)
Note: Author’s report that Suprasternal notch on right side with pressure was later removed from analysis since it was so bad – only 1/100 could be seen. There is also no data for the Suprasternal notch left and right without pressure – only a report of how often pressure improved the view.
The best images from each view were saved for review by blinded reviewer. Images deidentified and ensured to have no info about what technique was used. Sent in random order.
Time to locate airway anatomy was documented (max allowed was 30 seconds)
Second reviewer assessed all studies (blinded to first review).
Recorded all patients’ age, sex, height, and neck circumference.
Who did the ultrasounds?
Single investigator, fellow in emergency point of care ultrasound
Received training by 30 min lecture and 10 proctored scans (overall < 2 hours).
The Scan
Linear transducer

Transcricothyroid method: palpate cricothyroid membrane, transducer placed transversely, attempted to view vocal cords.
Suprasternal method: palpate sternal notch, place transducer at midline. Then apply firm pressure to the trachea. Then move the left and right of tracheal, obtaining images with and without pressure.
Endotracheal intubation on 5 Minute Sono
Results
The Patients
N = 100
- Ages 19-101, mean age 56
- BMI 14.8-44.1, mean weight 75 kg
- Mean neck circumference 38 cm
- 57% male
Primary Outcomes
Note: Numbers are slightly different in the table compared to what is reported in the text (these data are from the table)
Adequate visualization
Suprasternal to left with pressure was best – 92%
SSN with pressure – 81%
Transcricothyroid membrane – 78%
SSN without pressure – 52%
SSN to right of tracheal – 1%
Complete (not just adequate) visualization in SSN left with pressure was 46%.
Pressure improved views in 51%.
Moving to left improved view in 76%.
Odd ratios were probably not necessary but…
SSN + pressure on left had improved adequate visualization compared to SSN without pressure OR 10.3
SSN with pressure had improved adequate visualization compared to without pressure OR 4.1
Other Findings
Mean time was 9±7 seconds for TCM
6±7 seconds for SSN without pressure
8±6 for SSN with pressure
7±5 seconds for SSN with pressure to the left
*No statistically significant difference between times
Intraobserver agreement – Kappa 0.75
Limitations
Convenience sample.
Single skilled operator.
Who knows how this will perform in real life – in patients who are actually getting intubated. It is somewhat concerning that they could not visualize the structures in 8% of patients who were not even being intubated. Basically, these findings don’t necessary translate to the real deal. It might be hard to actually pick up on the intubation even when visualizing the appropriate anatomy. Or maybe patients getting intubated are inherently harder to find the anatomy. Placing pressure on the tracheal could make it harder to intubate. Basically, the next step after this study would be to confirm these results on patient’s getting intubated. Is this data vitally necessary to practice? – probably not.
Take Home Points
1. The best technique to visualize the tracheal and esophagus simultaneously is with the transducer to the left of the suprasternal notch using light pressure.
2. We don’t know if this holds true in patients who are actually getting intubated.
Our score