Authors: Olivia Victoriano, MD (EM Resident Physician, UHS SoCal MEC Emergency Medicine Residency, Temecula, CA); Jacob Avila, MD, RDMA (Core Faculty, UHS SoCal MEC Emergency Medicine Residency, Temecula, CA) // Reviewed by: Stephen Alerhand, MD (@SAlerhand); Brit Long, MD (@long_brit)
Case
An 86-year-old female with a history of osteoporosis and mild cognitive impairment presents to the emergency department for right hip pain after a fall from her bed at home. She has not been able to move her right hip since that time or put any weight on her right lower extremity. When she arrives at the ED, you notice that her right hip is held in an abducted and flexed position. Her right leg is rotated outward and appears shorter than the left leg. She has an ecchymotic area of the lateral aspect on the right thigh. X-ray imaging of the hip is ordered and shows a right-sided intertrochanteric fracture. The patient is clearly uncomfortable and shouting any time she is moved. Her current systolic blood pressure is hovering in the low 100’s and EMS reports that they administered 25 micrograms of fentanyl IV and she subsequently required 2L O2 nasal cannula to keep her oxygen saturation in the 90’s. On arrival to the ED, she immediately requests pain medicine.
What are some issues with parenteral opiates in the ED?
- Opiate use can cause delirium in the elderly, especially in those with baseline impaired cognition
- Opioids decrease respiratory drive (via the mu-opioid receptors in the CNS) which may cause hypoxia
- In addition to decrease in respiratory drive, opioids can cause other undesirable side effects such as oversedation
- Tolerance to opioids in chronic opioid users cause them to be less effective in the acute setting
- Opiate addiction is an ongoing public health crisis that necessitates utilization of alternative therapies for pain
Approach to Hip Fractures in the Elderly
Acute pain is the most common reason for visiting the emergency department. There is an association with treatment of pain and opiate use disorder which accounts for 5.8 million additional years lived with disability. Alternatives to opiates for the acute management of pain, such as local administration of topical anesthetic, can reduce opiate dependence and side effects. Additionally, local anesthetics in the treatment of pain decreases the incidence of systemic side effects, including effects on the central nervous system. Here we will outline treatment options for an acute hip fracture using local anesthetic administration.
Innervation of the proximal femur
The proximal femur has a relatively complex innervation, with contributions from the femoral nerve (FN), the obturator nerve (ON) and the sciatic nerves (SN).

While anesthetizing any of these nerves will be beneficial with regards to pain management, the goal should be to attempt to block the largest quantity of nerves. The hip blocks will block the ON and FN to variable degrees.
This guide will cover the infrainguinal fascia iliaca block, the suprainguinal fascia iliaca block and the pericapsular nerve group (PENG)
Fascia Iliaca Compartment Nerve Block
Indications: Hip and knee analgesia, anterior thigh analgesia (i.e. femur fractures, pubic ramus fractures, acetabular fractures and hip dislocations)
Contraindications: Anticoagulation (not including NSAIDs or aspirin), overlying cellulitis at site of needle insertion, or fractures at risk for compartment syndrome on the same extremity (i.e. tibial plateau fractures)
Advantages of this block: relatively far from critical vascular structures like the femoral artery (FA) and femoral nerve. In addition, the analgesic effect has been shown to be superior to parenteral opioids in alleviating pain with movement of the hip. This may aid in post-operative rehabilitation.
Distribution: FN ± lateral femoral cutaneous nerve and the ON.
Anesthetic distribution of fascia iliaca block. (NYSORA.com)
Equipment:
- Linear Ultrasound transducer (6-14 MHz) with sterile sleeve and sterile gel
- Two 20 mL syringes, or 60mL syringe
- 80-mm to 100-mm, 22-gauge nerve block needle
- Extension tubing to connect to syringe and nerve block needle (as shown below)
- 10mL syringe with 25 gauge needle for local wheal
- 30-40mL of dilute (0.25% of bupivacaine) long-acting anesthetic, making sure to not go over the maximum number of local anesthetic for the specific patient.
- 5mL of 1% lidocaine (for “skin wheal”)
- Sterile gloves
- Chlorhexadine
- Ideally, a secondary operator to help with administration of anesthetic

Syringe with nerve block needle set up (AliEM.com)
LANDMARKS, POSITIONING, AND TECHNIQUE
Infra-Inguinal Fascia Iliaca Nerve Block Approach
Patient will need to be lying in a supine position with the bed flattened. Ideally, you will position yourself and your equipment on the side of the affected extremity and the ultrasound machine on the contralateral side of the fracture to maintain appropriate line-of-sign between your needle/transducer and the ultrasound screen. Transducer will be placed on the inguinal crease in a transverse position. The FA will be identified as a pulsatile and the most medial neurovascular structure, bordered laterally by the femoral vein (FV). Lateral to the FV, a triangular structure will be seen, which represents the FN and a small bundle of adipose cells. Just superficial to the FN, a hyperechoic (white) line will be seen that represents the fascia iliaca.
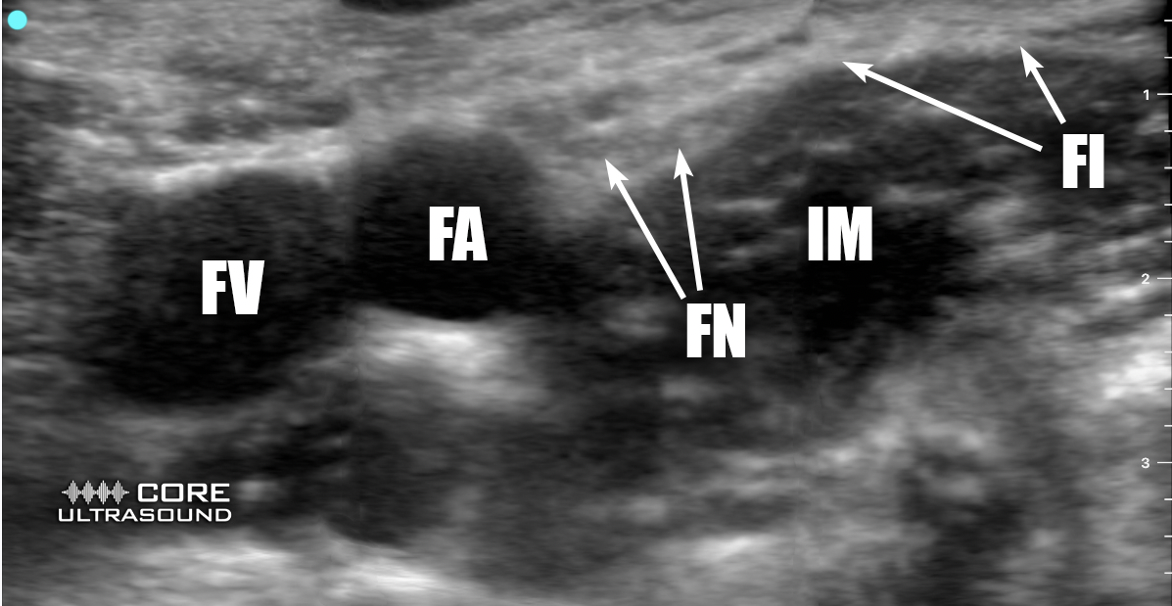
(FV = Femoral vein, FA = Femoral artery, FN = Femoral nerve, IM = Iliacus muscle, FI = Fascia iliaca)

Another visualization of landmarks for cognitive priming of infra-inguinal nerve block.
FA, femoral artery; FV, femoral vein; FN, femoral nerve; GnFN, genitofemoral nerve; LFcN, lateral femoral cutaneous nerve. (From Compendium of Regional Anesthesia)
The target for injection will the area just lateral to the FN, deep to the fascia iliaca and superficial to the iliacus muscle. Once you find the appropriate location for injection using ultrasound guidance, you will prep the patient in a sterile manner:
- Prepare your anesthetic mixture of bupivacaine in a 30 or 40 mL syringe.
- Clean the inguinal region with copious chlorhexidine and place sterile drape over the region of interest.
- Inject lidocaine as a skin wheal in the region where the injection will take place
- Don sterile glove and place the sterile ultrasound cover on the transducer.
- Attach the nerve block needle tubing to the syringe that an assistant is holding.
- Place the sterile ultrasound transducer over the area of interest once again, while holding the probe in your non-dominant hand and the needle in your dominant hand
- The needle should be placed in-line with the long-axis of the transducer. The angle of insertion should be around 45-60 degrees. As the needle advances into the patient, it should be visualized in the long axis with the ultrasound transducer. Care should be taken to always keep perfect visualization of the needle.
- The goal is for the needle tip to be JUST underneath the fascia iliaca (you usually will feel a pop, or change in resistance)
- Once you visualize the appropriate position of the needle tip, have the secondary operator introduce a small aliquot (~1mL) of the anesthetic to ensure you are in the correct position.
- If your positioning is correct, you will see hydrodissection, or clear separation between the fascia iliaca and the iliacus muscle
- Make the necessary adjustments if you are too inferior (in the iliacus muscle) or superior (above the level of the fascia)
- Always use negative pressure before inserting anesthetic to confirm you are not in a vascular structure
- Once in the appropriate position, instill the remainder of the 30-40mL of your anesthetic into the space (a volume of at least 30mL is generally necessary to accomplish appropriate “spread” within fascia iliaca)
- You want to see that the anesthetic is moving medially (toward the femoral nerve) and laterally (toward the sartorius muscle) in the same fascial plane.

(Example of an intra-inguinal fascia ilaca block. FV = Femoral vein, FA = Femoral artery, FN = Femoral nerve, LA = Local anesthetic, FI = Fascia iliaca)
For a video on the technique of performing a fascia iliaca block, check out this link.
Other types of nerve blocks are also available for providing analgesia for a proximal femur fracture. These include the suprainguinal fascia iliaca block and the PENG block
Suprainguinal Fascia Iliaca Nerve Block Approach
The suprainguinal approach may result in more proximal spread of the anesthetic and successful analgesia. A disadvantage of this approach is that it requires visualization of the internal oblique muscle, which may be smaller and more difficult to locate in the elderly population. In this approach, the position of the patient and equipment remains the same. You will even use the same initial approach to locate the iliacus muscle. At this point, you will begin to move the probe superiorly until you are above the inguinal canal and the ASIS. You will then rotate the probe marker 90 degrees so that it is pointing toward the umbilicus. You will see the sartorius and internal oblique form a “bowtie” with the iliacus in the middle and inferiorly.


Use the same approach as above, but your goal now will be the middle of the bowtie, under the fascia iliaca and above the iliacus muscle. with the exception of the ultrasound probe, which will be positioned in a parasagittal orientation, as illustrated above.

Cognitive priming for supra-inguinal fascia iliaca nerve block. (From Compendium of Regional Anesthesia)
PENG: Pericapsular Nerve Group block
The final technique we will talk about is the PENG block. This block is likely superior with regards to the other two blocks described, due to it’s more reliable penetration of the obturator nerve, its more motor-sparing effect and the fact that it may be beneficial in acetabular fractures, which are fractures that the fascia iliaca blocks don’t reliable anesthetize. The downside is that it can be more technically challenging to perform due to the depth at which the anesthetic needs to be distributed.
LANDMARKS, POSITIONING, AND TECHNIQUE
The patient, operator and probe placement will be similar to the previously described blocks. However, instead of the traditional linear transducer, a curvilinear transducer should be placed in a transverse orientation at the proximal thigh (probe marker to patient’s right). The transducer should then rotated 45 degrees such that it is parallel to the inguinal crease.
Operator must first identify the femoral artery and femoral head.

The transducer can then slide slowly in a cephalad direction until the ilium, anterior inferior iliac spine (AIIS) and iliopubic eminence (IPE). You will see the psoas tendon overlying the ilium. The target for administration of anesthetic will be the subfascial plane immediately overlying the ilium, deep to the psoas tendon.



After the identification of the appropriate landmarks, patient can be prepped in a sterile manner. This process will be similar as in the fascia iliaca blocks. The overall technique is similar, except for the fact that a longer nerve block needle (often 3 inches) will need to be used in order to reach the region of the pelvis deep to the psoas tendon.
- Using an in-plane technique in a lateral-to-medial direction, insert the nerve block needle until you visualize the needle tip deep to the psoas tendon until you contact the ilium
- Have the second operator insert 2cc of saline to confirm placement
- You should visualize the lifting of the psoas tendon off of the pelvic floor with local anesthetic administration.
- Make necessary adjustments if the liftin of the psoas tendon is not visualized.
- Remember to always use negative pressure to ensure your needle tip is not in the intravascular space
- Once you confirm placement, insert 30-40mL of the long acting anesthetic into the plane.
Additional reminders for nerve blocks
‘The target for the local anesthetic should not be the nerves themselves, but rather the fascial planes in which the nerve lie.
Adequate analgesia may take 30 minutes to 1 hour.
Always ensure that you have adequate positioning and view of landmarks before starting the procedure. Set the table before you eat!
Consistent needle visualization and landmark visualization throughout these dynamically-guided procedures is important to preventing accidental intramuscular injection (which can in turn cause femoral nerve blockade and reduction of motor function).
There are many anesthetics to choose from, but the best anesthetics to use in the case of an acute hip injury are long-acting. Always ensure that you correct for the patient’s weight when choosing an anesthetic and determining volume.

Local amide-based anesthetic agents and their pharmacokinetic effects, adapted from Goldfrank’s Toxicologic Emergencies (ACEP.org)
Case Resolution
Patient is reevaluated in the emergency department 40 minutes after the nerve block was performed. You have consulted orthopedic surgery, who is planning for operative repair. She is now having significant resolution of her pain and pending her operation.
Further Resources:
https://www.acep.org/emultrasound/newsroom/apr2021/pericapsular-nerve-group-peng-block-for-patients-with-hip-or-pelvis-fractures-in-the-ed/#:~:text=The%20pericapsular%20nerve%20group%20(PENG,accessory%20obturator%20nerve%20(AON).
https://www.aliem.com/fascia-iliaca-nerve-block/








1 thought on “Ultrasound-Guided Regional Anesthesia for Hip Fractures”
Pingback: Quiz 171, December 9, 2022 – The FOAMed Quiz